Abstract
Steroid therapy appeared to be a standard treatment for autoimmune pancreatitis (AIP), although some AIP patients improve spontaneously. The indications for steroid therapy in AIP patients are symptoms such as obstructive jaundice, abdominal pain, and back pain, and the presence of symptomatic extrapancreatic lesions. Before steroid therapy, jaundice should be managed by biliary drainage in patients with obstructive jaundice, and blood glucose levels should be controlled in patients with diabetes mellitus. For the initial oral prednisolone dose for induction of remission, 0.6 mg/kg/day is recommended. The initial dose is administered for 2–4 weeks, and the dose is tapered by 5 mg every 1–2 weeks, based on changes in the clinical manifestations, biochemical blood tests (such as liver enzymes and IgG or IgG4 levels), and repeated imaging findings (US, CT, MRCP, ERCP, etc.). The dose is tapered to a maintenance dose (2.5–5 mg/day) over a period of 2–3 months. Steroid therapy should be stopped based on the disease activity in each case. Stopping of maintenance therapy should be planned within at least 3 years in cases with radiological and serological improvement. Re-administration or dose-up of steroid is effective for treating AIP relapses. The prognosis of AIP appears to be good over the short-term with steroid therapy. It is unclear whether the long-term outcome is good because there are many unknown factors, such as relapse, pancreatic exocrine or endocrine dysfunction, and associated malignancy.
Similar content being viewed by others
CQ-III-1. Do AIP patients improve spontaneously?
-
Some AIP patients improve spontaneously. (Level of recommendation: B)
Swelling of the pancreas or irregular narrowing of the main pancreatic duct improves spontaneously without steroid therapy in some AIP patients. According to Wakabayashi et al. [1], pancreatic swelling was alleviated in 9 (24%) of 37 AIP patients with only conservative therapy, and of these, narrowing of the main pancreatic duct also improved after 3–60 months in 4 patients, remained unchanged in 3 patients, and worsened in 2 patients. It has been reported that most AIP patients who improved spontaneously did not have bile duct stenosis [2, 3]. According to Kamisawa et al. [2], in 21 AIP patients, spontaneous improvement was detected in 2 non-jaundiced patients (10%). Kubota et al. [3] compared the clinicopathological parameters in 8 AIP patients with remission in the absence of steroid therapy and 12 patients with remission after steroid therapy, and they found an association between remission in the absence of steroid therapy and seronegativity for IgG4, absence of obstructive jaundice, absence of diabetes mellitus, and the presence of focal pancreatic swelling.
Ozden et al. [4] reported an AIP patient who showed spontaneous regression of biliary obstruction 2 months after biliary drainage, and the drainage catheter was removed. Araki et al. [5] reported the natural course of an AIP patient in whom a mass in the uncinate process of the pancreas spontaneously decreased in size and disappeared after 9 months; conversely, however, the mass in the tail increased in size.
CQ-III-2. What are the indications for steroid therapy in AIP patients?
-
The indications for steroid therapy in AIP patients are symptoms such as obstructive jaundice, abdominal pain, and back pain, and the presence of symptomatic extrapancreatic lesions. (Level of recommendation: A)
According to the nationwide survey by the Research Committee of Intractable Pancreatic Diseases supported by the Ministry of Health, Labor, and Welfare of Japan [6], three quarters of all AIP patients received steroid therapy. The remission rate of steroid-treated AIP was 98%, which was significantly higher than that of patients without steroid therapy (88%), and the period necessary to achieve remission averaged 98 days in steroid-treated patients, which was significantly shorter than the average 142 days in patients without steroid therapy. Based on these findings, steroid therapy appeared to be a standard treatment for AIP.
Steroid therapy is effective for extrapancreatic lesions such as sclerosing cholangitis as well as the pancreatic lesion in AIP. AIP is frequently associated with stenosis of the bile duct due to sclerosing cholangitis, and obstructive jaundice is a frequent initial symptom. As 91% of AIP patients with obstructive jaundice underwent steroid therapy according to the nationwide survey [6], obstructive jaundice is the principal indication for steroid therapy [2, 6–10]. AIP patients rarely have the severe abdominal pain that occurs in acute pancreatitis, but persistent abdominal or back pain in AIP appears to be an indication for steroid therapy [2, 6–9]. Associated symptomatic extrapancreatic lesions, such as retroperitoneal fibrosis, interstitial pneumonia, tubulointerstitial nephritis, and hepatic or pulmonary pseudotumor, are indications for steroid therapy [2, 7, 9, 10].
As impaired pancreatic endocrine or exocrine function improved in some AIP patients, marked impairment of pancreatic endocrine or exocrine function may be one of the indications for steroid therapy [7, 10, 11]. Some AIP patients showing diffuse enlargement of the pancreas undergo steroid therapy even if they are asymptomatic [2, 9]. It may be better to follow up for 1–2 weeks before starting steroids in order to check for spontaneous regression. In principle, steroid therapy should be performed for patients diagnosed as having AIP, but a facile steroid trial to differentiate AIP from pancreatic cancer should be prohibited [12].
CQ-III-3. How do we perform initial steroid therapy?
-
Before steroid therapy, jaundice should be managed by biliary drainage in patients with obstructive jaundice, and blood glucose levels should be controlled in patients with diabetes mellitus. For the initial oral prednisolone dose for induction of remission, 0.6 mg/kg/day is recommended. The initial dose is administered for 2–4 weeks and then gradually tapered. (Level of recommendation: B)
Before steroid therapy, it is important to distinguish AIP from pancreatic or biliary cancer with imaging studies and an endoscopic approach [9].
In cases with obstructive jaundice due to bile duct stenosis, endoscopic or transhepatic biliary drainage is performed. Cytologic examination of the bile is performed repeatedly. After cytologic examination, a plastic stent is sometimes inserted. Steroid therapy can be started without biliary drainage in cases with mild jaundice. Blood glucose levels should be controlled in patients with diabetes mellitus before steroid therapy [8, 9].
According to the nationwide survey by the Research Committee of Intractable Pancreatic Diseases [6], the initial oral prednisolone dose was 30 mg/day (n = 54) or 40 mg/day (n = 32) in 93 AIP patients treated with steroids. The period necessary to achieve remission from the start of initial administration averaged 70 days in patients treated with an initial prednisolone dose of 30 mg/day, which was not significantly different from the period (average 91 days) in those treated with an initial prednisolone dose of 40 mg/day. There were no significant differences in the initial prednisolone dose administered to AIP patients with obstructive jaundice between patients treated with steroids alone [0.60 ± 0.12 mg/kg/day (mean ± SD)] and those treated with biliary drainage and steroids (0.60 ± 0.17 mg/kg/day). A recent multicenter study showed similar results [9]. Given these findings, the recommended initial oral prednisolone dose is 0.6 mg/kg/day, and it should be gradually tapered after 2–4 weeks of administration [9].
In western countries, it has been reported that AIP patients are treated with an initial prednisolone dose of 50–75 mg/day [13], 40 mg/day [14, 15], or 0.5 mg/kg/day [16]. Matsushita et al. [17] reported that steroid pulse therapy is useful and may prevent unnecessary surgery when oral steroid therapy is not indicated because of the required period for drug tapering.
CQ-III-4. How is the dose of steroid tapered?
-
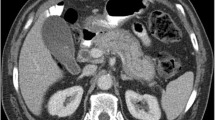
After 2–4 weeks at the initial dose, the dose is tapered by 5 mg every 1–2 weeks, based on changes in the clinical manifestations, biochemical blood tests (such as liver enzymes and IgG or IgG4 levels), and repeated imaging findings (US, CT, MRCP, ERCP, etc.). The dose is tapered to a maintenance dose over a period of 2–3 months. (Level of recommendation: B)
In order to induce remission, after 2–4 weeks at the initial dose, the dose is tapered by 5 mg every 1–2 weeks, based on changes in clinical manifestations, biochemical blood tests (such as liver enzymes and IgG or IgG4 levels), and repeated imaging findings (US, CT, MRCP, ERCP, etc.). The dose is tapered gradually to a maintenance dose, usually 5–10 mg/day [6, 8, 9, 18] (Fig. 1). After 15 mg/day, the dose is tapered more gradually, and the amount of steroid is reduced to a maintenance dose over a period of 3–6 months [9].
Regimen of oral steroid therapy for AIP. Ref. [25] is partially modified
At the Mayo Clinic, an initial prednisolone dose of 40 mg/day was administered for 4 weeks, followed by tapering of 5 mg per week (total of 11 weeks of treatment) [14]. According to Park et al. [16] in Seoul, the induction dosage of prednisolone was initially administered at 0.5 mg/kg/day for 1–2 months and was gradually reduced by 5–10 mg per month to the maintenance dose, and maintenance therapy stopped completely after an average period of 6 months.
Because radiological improvement appears 1–2 weeks after the start of steroid therapy, morphological and serological evaluation for effectiveness of steroid therapy should be performed 1–2 weeks after starting steroid therapy. A poor response to steroid therapy should raise the possibility of pancreatic cancer and the need for re-evaluation of the diagnosis [9].
CQ-III-5. Is maintenance steroid therapy necessary?
-
To prevent relapse, maintenance therapy (2.5–5 mg/day) is recommended. (Level of recommendation: B)
There have been no prospective studies on the necessity of maintenance therapy in steroid therapy for AIP. In Japan, steroid therapy is usually stopped after some period of maintenance therapy. The relapse rate of AIP during or after steroid therapy is reported to be 10% (4/41) [10] to 53% (16/30) [20].
At the Mayo Clinic, initial steroid therapy finished after 11 weeks, and maintenance therapy was not performed. Under this regimen, 16 (53%) of 30 AIP patients associated with sclerosing cholangitis relapsed within median 3 months (0–14 months) after therapy, and this rate did not differ from the relapse rate in surgically treated patients (44%; 8/18) [20].
According to the survey by the Research Committee of Intractable Pancreatic Diseases [21], 38 (40%) of 96 AIP patients who underwent maintenance therapy relapsed, and of these, relapse occurred only in the pancreas in 19 (50%), only in extrapancreatic lesions in 11 (29%), and in both lesions in 8 (21%). The relapse rate of patients during maintenance therapy with prednisolone of more than 5 mg/day was 26% (10/38), which was significantly lower than the rate (54%, 14/26) in patients who stopped maintenance therapy (p < 0.05) (Fig. 2).
Based on these findings, maintenance steroid therapy appears to be effective in preventing AIP relapse. As the anti-inflammatory and immunosuppressive effects of steroids appear to suppress the activity of AIP, maintenance therapy by prednisolone by at least 5 mg/day is recommended. However, as some patients do not relapse without maintenance therapy, and some patients relapse during steroid tapering [20, 22] or during maintenance therapy with relatively high doses of prednisolone, in order to judge the indications of maintenance therapy, it is important to evaluate disease activity in the patient. The Research Committee of Intractable Pancreatic Diseases compared the clinical features of patients with and without relapse, and reported that the clinical features of patients who tended to relapse included pancreatic enlargement of more than one-third of the entire pancreas, association with extrapancreatic lesions diagnosed by Gallium scintigraphy, and association with extrapancreatic sclerosing cholangitis [21]. In a Mayo Clinic report [20], the presence of proximal extrahepatic/intrahepatic strictures was predictive of relapse in AIP patients with sclerosing pancreatitis. Hirano et al. [19] also reported that obstructive jaundice at onset was a significant predictive factor for relapse of AIP.
CQ-III-6. When should steroid therapy be stopped?
-
Steroid therapy should be stopped based on the disease activity in each case.
-
Stopping of maintenance therapy should be planned within at least 3 years, in cases with radiological and serological improvement. (Level of recommendation: I)
There is no consensus about the duration of steroid therapy in AIP patients. According to Kamisawa et al. [10], steroid medication was stopped an average of 19.5 months after the start of steroid therapy in 9 patients with complete morphological and serological resolution, and none of these patients relapsed.
According to the survey by the Research Committee of Intractable Pancreatic Diseases [21], most patients relapsed within 3 years from the start of steroid therapy (Fig. 3). In those patients relapsing after 3 years, the incidence of patients stopping steroid therapy was higher than that of cases during maintenance therapy. There were no differences in the period of steroid therapy between relapsed cases after stopping steroid therapy (12.8 ± 8.9 months, 1–30 months, n = 14) and non-relapsed cases after stopping steroid therapy (13.5 ± 10.5 months, 1–31 months, n = 11).
Maintenance therapy is effective to prevent relapse. However, since AIP patients are typically elderly and are at high risk of developing steroid-related complications, such as osteoporosis and diabetes mellitus, cessation of the medication should be attempted. Cessation of maintenance therapy should be planned within at least 3 years, in cases with radiological and serological improvement. When stopping medication, it is necessary to evaluate disease activity. After stopping medication, patients should be followed up for relapse of AIP [9, 21].
CQ-III-7. Is early prediction of AIP relapse possible?
-
In patients with a relapse of AIP, pancreatic enlargement on imaging, elevated serum IgG4 levels, elevated serum hepatobiliary and pancreatic enzymes, re-appearance of extrapancreatic lesions, elevated soluble IL-2 receptor or immune complex, and consumption of complement are detected. (Level of recommendation: B)
The Research Committee of Intractable Pancreatic Diseases evaluated disease activity of AIP using score. Scores took into account enlargement of the pancreas, serum levels of γ-globulin, IgG and IgG4, presence of autoantibodies, elevated serum levels of hepatobiliary enzymes, elevated or decreased serum levels of pancreatic enzymes, impaired pancreatic exocrine function, associations with various extrapancreatic lesions, diabetes mellitus, and other autoimmune diseaseS, elevated serum β-2 microglobulin or soluble IL-2 receptor, complement consumption, and elevation of immune complexes. Score of AIP activity was 12.2 before steroid therapy and decreased to 1.83 after steroids. These findings suggest that the scoring system reflects disease activity of AIP. However, it is unclear whether the system can predict early AIP relapse. Cutoff values suggesting relapse are also unknown [23].
CQ-III-8. How are AIP relapses treated?
-
Re-administration or dose-up of steroid is effective for treating AIP relapses.
-
Remission can be obtained with the same prednisolone dose as the initial dose in most relapsed AIP cases, but it may be necessary to taper more gradually. (Level of recommendation: I)
Remission can be obtained with re-administration or dose-up of steroid in most relapsed AIP cases. According to Kamisawa et al. [10], 4 AIP patients who relapsed at pancreatic or extrapancreatic lesions during maintenance therapy obtained remission with dose-up (30 mg/day) of steroid. Nishino et al. reported that bile duct stenosis and swelling of the salivary glands relapsed during steroid tapering in 1 and 3 patients respectively, but they improved with dose-up steroid. They also tapered the steroid more gradually (1 mg/2 weeks) as compared with the speed of initial therapy in relapsed cases [22]. At the Mayo Clinic, second relapse occurred in 4 of 11 patients with first relapse, despite slow steroid tapering after the second induction therapy. They also reported that immunomodulatory drugs such as azathioprine (initial dose of 50 mg/day, increasing to 2–2.5 mg/kg) and mycophenolate mofetil (initial dose of 500 mg twice daily, increasing to 750 mg twice daily) were effective in 7 relapsed AIP patients, and none of these patients relapsed (median follow-up period on immunomodulatory drugs alone, 6 months; range, 2–19 months) [20]. Although immunomodulatory drugs appear to prevent relapse and to maintain remission, indications for these drugs should be judged carefully based on their adverse effects.
CQ-III-9. Do pancreatic exocrine and endocrine functions improve after steroid therapy in AIP patients?
-
Pancreatic exocrine and endocrine functions improve after steroid therapy in some AIP patients. Many AIP patients with type 2 diabetes mellitus before AIP onset showed worsening of diabetes mellitus control after steroid therapy. (Level of recommendation: A)
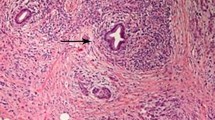
Many AIP patients have associated pancreatic exocrine and endocrine dysfunction [2, 7, 11, 24–26]. It has been reported that improvement of pancreatic exocrine and endocrine function was detected after steroid therapy in 38% [22] to 50% [25] and 25% [22] to 45% [25] of AIP patients, respectively. It has also been suggested as a mechanism of improvement in pancreatic exocrine and endocrine functions after steroid therapy that steroid suppresses lymphoplasmacytic cell infiltration and fibrosis, permitting the attenuation of blood flow [26] and further regenerating islet cells by suppression of cytokine production [27]; however, the precise mechanisms remain unclear.
Diabetes mellitus control worsens in 75% of AIP patients with type 2 diabetes mellitus before AIP onset after steroid therapy [25]. DM also develops after steroid therapy in some AIP patients [24, 25]. We should therefore take occurrence of DM into consideration in patients who continuously undergo steroid therapy.
CQ-III-10. Is the prognosis of AIP good?
-
The prognosis of AIP appears to be good over the short-term with steroid therapy.
-
It is unclear whether the long-term outcome is good, because there are many unknown factors, such as relapse, pancreatic exocrine or endocrine dysfunction, and associated malignancy. (Level of recommendation: B)
The relapse rate of AIP is reported to be 10% [10] to 53% [20] in patients treated with steroids, and 28% [28] to 35% [20] in those without steroid therapy.
AIP responds well to steroid therapy, and remission can be induced in most AIP patients. However, with respect to the long-term outcome, there are many unknown factors, such as relapse, pancreatic exocrine or endocrine dysfunction, and associated malignancy.
Nishino et al. [22] reported that pancreatic atrophy developed in 33% of 12 patients, and 1 patient developed early gastric cancer after 29 months of steroid therapy, while another patient developed advanced rectal cancer after 13 months of steroid therapy. According to Hirano et al., unfavorable events occurred in 32% of AIP patients treated with steroid therapy during an average 41-month follow-up period, and they occurred in 70% of those without steroid therapy during an average follow-up of 61 months. Furthermore, 1 patient treated with steroid therapy died of acute myelocytic leukemia, 1 patient not treated with steroid therapy died of lung cancer, and 1 patient not treated with steroid therapy died of pancreatic cancer [19]. Kubota et al. [3] also reported 4 patients who were diagnosed as having a malignancy during follow-up (pancreatic cancer, n = 2; breast cancer, n = 2; gastric cancer, n = 1). Kamisawa et al. [10] reported that marked atrophy of the pancreas was observed in 30% of AIP patients during follow-up. Park et al. [16] reported that 13 (33%) of 40 patients treated with steroids relapsed during a median follow-up period of 40 months, with 7 relapsing on the maintenance dose of prednisolone (2.5–7.5 mg/day), and the remaining 6 patients relapsing while off steroids. According to Ghazale et al. [20], 16 (53%) of 30 patients treated with steroids relapsed during a median follow-up period of 30 months. They also reported that 7 of 53 AIP patients died and that pancreatic cancer and metastatic pancreatic cancer developed.
In 37 AIP patients who underwent pancreatoduodenectomy, no patients relapsed during a median follow-up period of 33 months, and 68% subjectively rated their quality of life as better [29]. On the other hand, among 29 surgically resected AIP patients, 8 (28%) relapsed at a median time to recurrence of 11 months during a median follow-up period of 38 months [28]. Schneldorfer et al. [30] reported that in 8 surgically resected AIP patients, improved quality of life (QOL) was seen in almost half of patients, but 2 (25%) patients relapsed.
CQ-III-11. Is there any relationship between AIP and pancreatic cancer?
-
There are a few papers reporting an AIP case developing pancreatic cancer, but it is unclear whether there is a relationship between AIP and pancreatic cancer. (Level of recommendation: B)
It has been reported that chronic pancreatitis is one of the risk factors for pancreatic cancer [31]. It has been reported that some AIP patients developed pancreatic atrophy or pancreatic stones [32, 33]. AIP occurred predominantly in the elderly males. It is necessary to observe whether there is an association with pancreatic cancer and other malignancies in AIP patients treated with steroid for a long period, since steroid therapy is immunosuppressive. Periodic checks of serum tumor markers are necessary during follow-up.
There have been 6 recent papers reporting AIP cases developing pancreatic cancer [34–39]. The locations of these cancers were the pancreatic head (n = 1), body (n = 3), and tail (n = 2). All patients were males, and average age was 72 years (62–80 years). Three pancreatic cancers were diagnosed simultaneously with AIP, and the other 3 cancers were diagnosed 3–5 years after the onset of AIP. Kamisawa et al. [40] reported frequent and significant K-ras mutations in the pancreas of AIP patients. However, it is unclear whether there is a relationship between AIP and pancreatic cancer.
References
Wakabayashi T, Kawaura Y, Satomura Y, Watanabe H, Motoo Y, Sawabu N. Long-term prognosis of duct-narrowing chronic pancreatitis. Strategy for steroid treatment. Pancreas. 2005;30:31–9.
Kamisawa T, Yoshiike M, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Treating patients with autoimmune pancreatitis: results from a long-term follow-up study. Pancreatology. 2005;5:234–40.
Kubota K, Iida H, Fujisawa T, Yoneda M, Inamori M, Abe Y, et al. Clinical factors predictive of spontaneous remission or relapse in cases of autoimmune pancreatitis. Gastrointest Endosc. 2007;66:1142–51.
Ozden I, Dizdaroglu F, Poyanli A, Emre A. Spontaneous regression of a pancreatic head mass and biliary obstruction due to autoimmune pancreatitis. Pancreatology. 2005;5:300–3.
Araki J, Tsujimoto F, Ohta T, Nakajima Y. Natural course of autoimmune pancreatitis without steroid therapy showing hypoechoic masses in the uncinate process and tail of the pancreas on ultrasonography. J Ultrasound Med. 2006;25:1063–7.
Nishimori I, Okazaki K, Kawa S, Otsuki M. Treatment for autoimmune pancreatitis. J Biliary Tract Pancreas (in Japanese). 2007;28:961–6.
Kamisawa T, Okamoto A. Autoimmune pancreatitis: proposal of IgG4-related sclerosing disease. J Gastroenterol. 2006;41:613–25.
Nishimori I, Okazaki K, Suda K, Kawa S, Kamisawa T, Tanaka S, et al. Treatment for autoimmune pancreatitis. Consensus of treatment for autoimmune pancreatitis by the Research Committee of Intractable Pancreatic Diseases supported by Ministry of Health, Labour and Welfare of Japan. Suizou (in Japanese). 2005;20:343–8.
Kamisawa T, Shimosegawa T, Okazaki K, Nishino T, Watanabe H, Kanno A, et al. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009;58:1504–7.
Kamisawa T, Okamoto A, Wakabayashi T, Watanabe H, Sawabu N. Appropriate steroid therapy for autoimmune pancreatitis based on long-term outcome. Scand J Gastroenterl. 2008;43:609–13.
Kamisawa T, Egawa N, Inokuma S, Tsuruta K, Okamoto A, Kamata N, et al. Pancreatic endocrine and exocrine function and salivary gland function in autoimmune pancreatitis before and after steroid therapy. Pancreas. 2003;27:235–8.
Okazaki K, Kawa S, Kamisawa T, Naruse S, Tanaka S, Nishimori I, et al. Clinical diagnostic criteria of autoimmune pancreatitis: revised proposal. J Gastroenterol. 2006;41:626–31.
Pearson RK, Longnecker DS, Chari ST, Smyrk TC, Okazaki K, Frulloni L, et al. Controversies in clinical pancreatology. Autoimmune pancreatitis: does it exist? Pancreas. 2003;27:1–13.
Ghazale A, Chari ST. Optimising corticosteroid treatment for autoimmune pancreatitis. Gut. 2007;56:1650–2.
Finkelberg DL, Sahani D, Deshpande V, Brugge WR. Autoimmune pancreatitis. N Engl J Med. 2006;355:2670–6.
Park DH, Kim MH, Oh HB, Kwon OJ, Choi YJ, Lee SS, et al. Substitution of aspartic acid at position 57 of the DQβ1 affects relapse of autoimmune pancreatitis. Gastroenterology. 2008;134:440–6.
Matsushita M, Yamashina M, Ikeura T, Shimatani M, Uchida K, Takaoka M, et al. Effective steroid pulse therapy for the biliary stenosis caused by autoimmune pancreatitis. Am J Gastroenterol. 2007;102:220–1.
Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Morphological changes after steroid therapy in autoimmune pancreatitis. Scand J Gastroenterol. 2004;11:1154–8.
Hirano K, Tada M, Isayama H, Yagioka H, Sasaki T, Kogure H, et al. Long-term prognosis of autoimmune pancreatitis with and without corticosteroid treatment. Gut. 2007;56:1719–24.
Ghazale A, Chari ST, Zhang L, Smyrk TC, Takahashi N, Levy MJ, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008;134:706–15.
Nishimori I, Otsuki M. Study about steroid therapy for autoimmune pancreatitis. Annual reports of Research Committee of Intractable Pancreatic Diseases supported by Ministry of Health, Labour and Welfare of Japan (in Japanese). 2008;137–44.
Nishino T, Toki F, Oyama H, Shimizu K, Shiratori K. Long-term outcome of autoimmune pancreatitis after oral prednisolone therapy. Intern Med. 2006;45:497–501.
Okazaki K, Nichimori I, Uchida K, Otsuki M. Study about indication of therapy and relapse in autoimmune pancreatitis—therapeutic effect and evaluation method of disease activity. Annual reports of the Research Committee of Intractable Pancreatic Diseases supported by Ministry of Health, Labour and Welfare of Japan (in Japanese). 2008;133–6.
Nishimori I, Tamakoshi A, Kawa S, Tanaka S, Takeuchi K, Kamisawa T, et al. Influence of steroid therapy on the course of diabetes mellitus in patients with autoimmune pancreatitis: findings from a nationwide survey in Japan. Pancreas. 2006;32:244–8.
Ito T, Nishimori I, Inoue N, Kawabe K, Gibo J, Arita Y, et al. Treatment for autoimmune pancreatitis: consensus on the treatment for patients with autoimmune pancreatitis in Japan. J Gastroenterol. 2007;42(Suppl 18):50–8.
Ito T, Kawabe K, Arita Y, Hisano T, Igarashi H, Funakoshi A, et al. Evaluation of pancreatic endocrine and exocrine function in patients with autoimmune pancreatitis. Pancreas. 2007;34:254–9.
Tanaka S, Kobayashi T, Nakanishi K, Okubo M, Murase T, Hashimoto M, et al. Corticosteroid-responsive diabetes mellitus associated with autoimmune pancreatitis. Lancet. 2000;356:910–1.
Weber SM, Cubukcu-Dimopulo O, Palesty JA, Suriawinata A, Klimstra D, Brennan MF, et al. Lymphoplasmacytic sclerosing pancreatitis: inflammatory mimic of pancreatic carcinoma. J Gastrointest Surg. 2003;7:129–37.
Hardacre JM, Iacobuzio-Donahue CA, Sohn TA, Abraham SC, Yeo CJ, Lillemoe KD, et al. Results of pancreaticoduodenectomy for lymphoplasmacytic sclerosing pancreatitis. Ann Surg. 2003;237:853–9.
Schnelldorfer T, Lewin DN, Adams DB. Long-term results after surgery for autoimmune sclerosing pancreatitis. J Gastrointest Surg. 2007;11:56–8.
Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW, Lankisch PG, Andersen JR, et al. Pancreatitis and the risk of pancreatic cancer. N Engl J Med. 1993;328:1422–7.
Takayama M, Hamano H, Ochi Y, Saegusa H, Komatsu K, Muraki T, et al. Recurrent attacks of autoimmune pancreatitis result in pancreatic stone formation. Am J Gastroenterol. 2004;99:932–7.
Kamisawa T, Okamoto A. Prognosis of autoimmune pancreatitis. J Gastroenterol. 2007;42(Suppl 18):59–62.
Inoue H, Miyatani H, Sawada Y, Yoshida Y. A case of pancreatic cancer with autoimmune pancreatitis. Pancreas. 2006;33:208–9.
Fukui T, Mitsuya T, Takaoka M, Uchida K, Matsushita M, Okazaki K. Pancreatic cancer associated with autoimmune pancreatitis in remission. Intern Med. 2008;47:151–5.
Ghazale A, Chari S. Is autoimmune pancreatitis a risk factor for pancreatic cancer? Pancreas. 2007;35:376.
Witkiewicz AK, Kennedy EP, Kennedy L, Yeo CJ, Hruban RH. Synchronous autoimmune pancreatitis and infiltrating pancreatic ductal adenocarcinoma: case report and review of the literature. Hum Pathol. 2008;39:1548–51.
Sakashita F, Tanahashi T, Yamaguchi K, Osada S, Sugiyama Y, Adachi Y. Case of pancreatic tail cancer associated with autoimmune pancreatitis. Jpn J Gastroenterol Surg. 2006;39:78–83.
Iida H, Kubota K, Mawatari H, Yoneda M, Goto A, Abe Y, et al. A case of autoimmune pancreatitis developed pancreatic tail cancer. Suizou. 2008;23:608–14.
Kamisawa T, Tsuruta K, Okamoto A, Horiguchi S, Hayashi Y, Xun X, et al. Frequent and significant K-ras mutation in the pancreas, the bile duct, and the gallbladder in autoimmune pancreatitis. Pancreas. 2009;38:890–5.
Acknowledgments
This study was supported by the grant-in-aid for the Refractory Pancreatic Disease from the Ministry of Labor, Health, and Welfare of Japan.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This article is the third of a three-article series on the Japanese consensus guidelines. The first and second articles are available at doi:10.1007/s00535-009-0184-x and doi:10.1007/s00535-009-0197-5, respectively. Names of committee members are provided in the first article.
Rights and permissions
About this article
Cite this article
Kamisawa, T., Okazaki, K., Kawa, S. et al. Japanese consensus guidelines for management of autoimmune pancreatitis: III. Treatment and prognosis of AIP. J Gastroenterol 45, 471–477 (2010). https://doi.org/10.1007/s00535-010-0221-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0221-9