Abstract
Introduction
Asymptomatic erosive esophagitis is a common yet rarely reported disease. The purpose of this study is to investigate the prevalence of asymptomatic erosive esophagitis and to identify the risk factors for this disease.
Materials and Methods
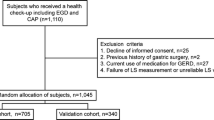
In this study, we investigated 572 asymptomatic subjects undergoing health check-ups after upper gastrointestinal endoscopy. The severity of esophagitis was evaluated by the Los Angeles classification, and the independent risk factors for asymptomatic esophagitis were analyzed by the logistic regression method.
Results
The results showed the prevalence of erosive esophagitis in asymptomatic subjects was 12% (70/572). In all asymptomatic subjects, erosive esophagitis was grade A (71%) or B (29%). Univariate analysis revealed that male gender, high body mass index (BMI), and consumption of tobacco, alcohol, tea, spicy foods, and betel nut were associated with the development of erosive esophagitis. Multivariate analysis revealed that male gender (OR, 3.8, 95% CI, 1.5–9.3) and high BMI (BMI 25–30: OR, 2.3, 95% CI, 1.3–4.2; BMI >30: OR, 3.8, 95% CI, 1.3–10.9) were independent predictors of erosive esophagitis.
Conclusion
Our data revealed male gender and high BMI are independent risk factors for asymptomatic erosive esophagitis.
Similar content being viewed by others
References
Fass R, Dickman R. Clinical consequences of silent gastroesophageal reflux disease. Curr Gastroenterol Rep. 2006;8:195–201.
El-Serag HB, Petersen NJ, Carter J, et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126:1692–1699.
Ohara S, Kouzu T, Kawano T, Kusano M. Nationwide epidemiological survey regarding heartburn and reflux esophagitis in Japanese. Jpn J Gastroenterol. 2005;102:1010–1024.
Hu WH, Wong WM, Lam CL, et al. Anxiety but not depression determines health care-seeking behaviour in Chinese patients with dyspepsia and irritable bowel syndrome: a population-based study. Aliment Pharmacol Ther. 2002;16:2081–2088.
Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ 3rd. Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259–1268.
Kennedy T, Jones R. The prevalence of gastroesophageal reflux symptoms in a UK population and the consultation behaviour of patients with these symptoms. Aliment Pharmacol Ther. 2000;14:1589–1594.
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920.
Lagergren J. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–831.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180.
Lee SJ, Song CW, Jeen YT, et al. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001;16:373–376.
Manabe N, Yoshihara M, Sasaki A, Tanaka S, Haruma K, Chayama K. Clinical characteristics and natural history of patients with low-grade reflux esophagitis. J Gastroenterol Hepatol. 2002;17:949–954.
Nozu T, Komiyama H. Clinical characteristics of asymptomatic esophagitis. J Gastroenterol. 2008;43:27–31.
Nocon M, Labenz J, Jaspersen D, et al. Association of body mass index with heartburn, regurgitation and esophagitis: results of the progression of gastroesophageal reflux disease study. J Gastroenterol Hepatol. 2007;22:1728–1731.
El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–1250.
Hampell H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211.
El-Serage HB, Ergun GA, Pandolfino J, Fitzgerald S, Tran T, Kramer JR. Obesity increases oesophageal acid exposure. Gut. 2007;56:749–755.
Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo CA. Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med. 2006;354:2340–2348.
Sheu BS, Chang WL, Cheng HC, Kao AW, Lu CC. Body mass index can determine the healing of reflux esophagitis with Los Angeles Grades C and D by esomeprazole. Am J Gastroenterol. 2008;103:2209–2214.
Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD. Gastro-oesophageal reflux disease in obesity: pathophysiological and therapeutic considerations. Obes Rev. 2002;3:9–15.
Wisén O, Rössner S, Johansson C. Gastric secretion in massive obesity. Evidence for abnormal response to vagal stimulation. Dig Dis Sci. 1987;32:968–972.
Mercer CD, Wren SF, DaCosta LR, Beck IT. Lower esophageal sphincter pressure and gastroesophageal pressure gradients in excessively obese patients. J Med. 1987;18:135–146.
Kim N, Lee SW, Cho SI, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2007;27:173–185.
Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456.
Adeniyi KO, Olowookorun MO. Influence of sex on gastric acid secretion and parietal cell mass in the rat. Acta Physiol Hung. 1989;4:63–67.
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut. 2004;53:1730–1735.
Nocon M, Labenz J, Willicj SN. Lifestyle factors and symptoms of gastro-oesophageal reflux—a population-based study. Aliment Pharmacol Ther. 2006;23:169–174.
Dore MP, Maragkoudakis E, Fraley K, et al. Diet, lifestyle and gender in gastro-oesophageal reflux disease. Dig Dis Sci. 2008;53:2027–2032.
Conflict of Interest Disclosure
The authors have no conflicts of interest to declare.
Financial Support
The authors have received no funding and confirm there were no financial arrangements that could influence this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, FW., Tu, MS., Chuang, HY. et al. Erosive Esophagitis in Asymptomatic Subjects: Risk Factors. Dig Dis Sci 55, 1320–1324 (2010). https://doi.org/10.1007/s10620-009-0888-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0888-z