Abstract
Background:
Breast cancer becomes lethal when visceral metastases develop. At this stage, anti-cancer treatments aim at relieving symptoms and delaying death without resulting in additional toxicity. On the basis of their differential anti-oxidant defence level, tumour cells can be made more sensitive to chemotherapy than non-tumour cells when membrane lipids are enriched with docosahexaenoic acid (DHA), a peroxidisable and oxidative-stress-inducing lipid of marine origin.
Methods:
This open-label single-arm phase II study evaluated the safety and efficacy (response rate), as primary end points, of the addition of 1.8 g DHA daily to an anthracycline-based chemotherapy (FEC) regimen in breast cancer patients (n=25) with rapidly progressing visceral metastases. The secondary end points were time to progression (TTP) and overall survival (OS).
Results:
The objective response rate was 44%. With a mean follow-up time of 31 months (range 2–96 months), the median TTP was 6 months. Median OS was 22 months and reached 34 months in the sub-population of patients (n=12) with the highest plasma DHA incorporation. The most common grade 3 or 4 toxicity was neutropaenia (80%).
Conclusion:
DHA during chemotherapy was devoid of adverse side effects and can improve the outcome of chemotherapy when highly incorporated. DHA has a potential to specifically chemosensitise tumours.
Similar content being viewed by others
Main
Breast cancer is the most frequent cancer in women, with an incidence of >1 million new cases in the world in 2002, with 360 000 cases in Europe (http://www-dep.iarc.fr/). A significant proportion of patients die because of the development of metastases. At this stage, survival length and quality of life depend on disease sensitivity to anti-cancer treatments. Despite the advent of innovative approaches, current treatments still rely heavily on conventional chemotherapy. Efficacy of chemotherapy is usually dose dependent. Dose is limited by side effects as a consequence of toxicity to non-tumour tissues, which results from the poor selectivity of anti-cancer drugs for tumours. Thus, any approach aimed at increasing tumour sensitivity to chemotherapy while not affecting non-tumour tissues has a potential to improve metastatic breast cancer prognosis and clinical outcome.
Several research groups, including ours, have shown that docosahexaenoic acid (DHA), a lipid of marine algal origin mainly provided by diet, has, experimentally, the ability to increase the efficacy of anti-cancer agents. This highly unsaturated fatty acid incorporates into cell membrane phospholipids, particularly in fast growing or proliferating cells such as tumour cells or tumour tissues, as tumour fatty acid composition is influenced by dietary lipids (Chajes et al, 1995). Using cultured breast cancer cell lines, it was reported that pre-enrichment of these cells with DHA enhanced their sensitivity to a variety of anti-cancer classes of drugs (Begin et al, 1986; Menendez et al, 2005; Wang et al, 2007) and more specifically to anthracyclines, an oxidative stress-inducing anti-cancer drug with a quinone structure (Germain et al, 1998; Mahéo et al, 2005). Furthermore, a prolonged (several weeks) supplementation with DHA (fish oil or algae-derived DHA), initiated before and continued during chemotherapy, consistently increased the sensitivity of autochthonous mammary tumours to anti-cancer drugs (Shao et al, 1997; Hardman et al, 2001; Colas et al, 2005, 2006). Similar results have been observed with radiation therapy (Colas et al, 2004). This indicates that dietary DHA can make mammary tumours more sensitive to anti-cancer agents. DHA-induced tumour chemosensitisation or radiosensitisation was abolished by the concomitant addition of α-tocopherol, an anti-oxidant molecule (Colas et al, 2004, 2005) in a dose-dependent manner (Colas et al, 2006). With six double bonds, DHA is one of the most peroxidisable fatty acids and the increased sensitivity of tumour cells to chemotherapy may result in part from peroxidation of membrane-enriched DHA, as a consequence of the oxidative stress induced by anti-cancer drugs (Mahéo et al, 2005).
Several findings suggest that this increased sensitivity applies preferentially to aggressive tumour cells. We reported that cell defences against oxidative stress differ among cell lines, and found a deficiency in glutathion peroxidase induction by reactive oxygen species (ROS) in MDA-MB-231, a breast cancer cell line with particularly aggressive features, whereas MCF-7, a breast cancer cell line with less-advanced features of tumour progression, retained the complete set of anti-oxidant defences (Vibet et al, 2008). This indicates that the handling of ROS is altered along with tumour progression. As DHA incorporates into cell membranes, this differential handling of ROS may account for the selectivity of DHA-induced tissue sensitisation by anti-cancer agents in tumour tissues compared with non-tumour tissues. Along this line, the lack of additional toxicity in non-tumour tissues has been consistently documented under conditions in which tumour tissue DHA was sensitised to chemotherapy (Hardman et al, 1999; Kato et al, 2002; Germain et al, 2003; Xue et al, 2007) or radiation therapy (Wen et al, 2003) in rodents.
On the basis of these results, we conducted a pilot phase II clinical trial in metastatic breast cancer patients to investigate the efficacy and safety of adding DHA to an ROS-generating chemotherapy regimen, that is an anthracycline-based regimen (FEC). We found that the combination was safe while retaining significant anti-tumour activity in the sub-population of patients with high plasma DHA incorporation, suggesting that DHA has a potential to specifically chemosensitise tumours.
Materials and methods
Study design
This study aimed at investigating the efficacy and safety of the oral administration of DHA in breast cancer patients receiving an anthracycline-based chemotherapy as first-line therapy for metastases. It was designed as a prospective open-labelled phase II trial, performed in one single institution (University Hospital Bretonneau in Tours, France). Patients presenting with inclusion criteria were sequentially enrolled. The primary end points were response rate and safety profile. Secondary end points were time to progression (TTP) and overall survival (OS). The protocol was approved by the Tours University Hospital Ethic Committee in accordance with French law, and all patients signed an informed consent before inclusion.
Patient eligibility
Breast cancer patients with visceral metastases that were not amenable to hormonal therapy or alternative treatment and without earlier chemotherapy for metastases were eligible. Earlier adjuvant or neo-adjuvant therapy, with or without anthracyclines (maximum cumulative dose of ⩽250 mg m−2 for doxorubicin, 400 mg m−2 for epirubicin and 72 mg m−2 for mitoxanthrone), was allowed if completed at least 6 months before the study, as was adjuvant locoregional radiation therapy. Other criteria included age above 25 and below 75 years, Eastern Cooperative Oncology Group performance status (Oken et al, 1982) ⩽2 and life expectancy of at least 12 weeks. At least one bi-dimensionally measurable visceral lesion not located in fields irradiated in the earlier 4 months was required. Adequate bone marrow, renal and hepatic functions were required for study entry. Cardiac eligibility requirement was a left ventricular ejection fraction (LVEF) ⩾55%.
Patients were ineligible if they had a history of any other cancer (with the exception of non-melanoma skin cancer or cervical carcinoma in situ), bilateral (without other metastatic location) or inflammatory breast cancer. Patients included in any experimental study within the last 30 days were also excluded.
Treatments
To achieve a sufficient incorporation of DHA into tissue cell membrane phospholipids, an amount of 1.8 g/day of DHA was chosen on the basis of earlier studies carried out in healthy individuals and recently reviewed (Arterburn et al, 2006). DHA was provided as 0.5 g capsules of DHASCO containing DHA-enriched triglyceride oil of algal origin (44% DHA providing 0.2-g DHA). DHASCO capsules were kindly supplied by Martek Biosciences Corp. (Columbia, MD, USA). Patients received nine capsules of DHASCO daily (representing 200 mg × 9=1.800 mg DHA/day), as three capsules at each meal. DHA was administered from inclusion before initiation of chemotherapy (a 7–10-day loading period) and then for the 5 months of chemotherapy. Patients were explicitly asked to avoid any intake of anti-oxidants. They kept a daily record of their DHASCO intake, which was controlled every 3 weeks and further monitored by a capsule count at the end of the study. Compliance below 80% of the planned dose would have led to withdrawal of the patient from the study. FEC 75 chemotherapy, the standard of first-line chemotherapy in a metastatic setting at the time of accrual (Bonneterre et al, 2004), consisted of an intravenous infusion of cyclophosphamide (500 mg m−2), an i.v. bolus of fluorouracil (500 mg m−2), followed by an i.v. infusion of epirubicin (75 mg m−2). This treatment was administered on day 1 every 3 weeks. DHA was suspended on the day of chemotherapy administration. Duration was at least six cycles, except in the case of disease progression, unacceptable toxicity, patient refusal or any medical condition requiring study arrest. In case of a positive response after six cycles, treatment could be extended to nine cycles. Adjuvant or metastatic hormonal therapy was discontinued at study entry.
Patient monitoring, safety assessment and toxicity management
Complete clinical examination, biochemical analysis, electrocardiogram, cardiac sonography and pulmonary testing (spirometry, gas diffusion) were performed at baseline. Clinical examination and a biochemical analysis were repeated at day 1 of each cycle. Adverse events were graded according to the National Cancer Institute Common Toxicity Criteria (NCI-CTC, version 2.0, http://www.recist.com). Sonographic assessment of cardiac function was additionally performed by a single team of sonographists at the end of the study or when cardiac toxicity was suspected.
Treatment adaptation involved FEC regimen and not DHA. Dexamethasone and ondansetron were authorised anti-emetic drugs. Prophylactic granulocyte-colony-stimulating factor was authorised when required. Should a second episode of neutropaenia occur despite granulocyte-colony-stimulating factor, the dose of epirubicin would have to be reduced to 60 mg m−2. Dose delay to a maximum of 2 weeks was allowed in patients with an absolute neutrophil count of <1.5 × 109/l−1 and/or a platelet count of <100 × 109/−1 at day 22 (second cycle). Grades 3–4 non-haematological toxicity resistant to symptomatic treatment required epirubicin dose reduction to 60 mg/m2. If it was persistent despite dose reduction, patients were withdrawn from the study. Cessation of chemotherapy was required when signs of congestive heart failure occurred on the basis of functional criteria for cardiotoxicity or LVEF ⩽45%.
Tumour response and survival assessments
Assessement of tumour response through clinical and radiological evaluations was performed every two cycles, and compared with baseline. Imaging included computed tomography scans or abdominal sonography, bone scan, standard X-rays or magnetic resonance imaging, where appropriate. Response rate was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST version 1.0) guidelines (http://www.recist.com). Response was defined as complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD). The objective response rate (ORR) was defined as CR plus PR, divided by the number of patients. Clinical benefit was defined as the sum of CR, PR and SD, divided by the number of patients. Metastases-free interval was defined as the time from diagnosis of breast cancer to the first occurrence of metastasis. TTP was measured as the difference between time of response and time of disease progression. Thus, patients with no response were not included for calculation of TTP. OS was measured from inclusion into the trial to death from any cause, or censored as the date of last information when death was not recorded before the cutoff date (1 May 2009).
Measurements of plasma DHA
A mean number of six samples were obtained for each patient during the time course of the study. Venous blood was collected on EDTA and centrifuged at 900 g for 10 min to obtain plasma, which was divided into five aliquots and immediately stored at −20°C. At the time of analysis, an aliquot of each sample was unfrozen. Samples were analysed each day in batches of 24, in which patients were randomly distributed. Each sample was labelled with a code number that was blinded to the operators (ML and MP).
Plasma lipids were extracted with chloroform/methanol (2:1, vol/vol) (Folch et al, 1957). Phospholipids were purified with one-dimensional thin layer chromatography, transmethylated and fatty acid methyl esters analysed by gas chromatography on an AS 2000 gas chromatograph (ThermoFinnigan, Courtaboeuf Cedex, France) equipped with a cold on-column injector and a 60 m BPX 70 capillary column, with the aid of an automatic injector, under conditions as described earlier (Chajès et al, 1999). Peaks were identified by comparison of their retention times with those of authentic lipid standards (Supelco 37 Component FAME Mix, Sigma-Aldrich, Saint-Quentin Fallavier, France). Reproducibility of retention times was controlled by adding the standard before and after each batch. Fatty acid levels were calculated as percentages of total peak areas using ChromQuest software (ThermoFinnigan). Fatty acids were expressed as weight percentage (% of total peak area). Repeatability of the chromatography procedure was estimated from a sample earlier subdivided into 10 aliquots extracted and analysed on the same day. The coefficient of variations (CVs) of each fatty acid peak area was less than 0.5% for major peaks (such as 18:2 ω-6c, 18:1 ω-9c and 16:0) and not >10% for minor peaks, that is peaks <1% of total fatty acids.
Statistical considerations
Sample size and termination rules
A total of 25 patients were required to provide a 95% confidence interval (CI) ranging from 0.11 (no response) to 0.41 (12 or 13 responses). After Gehan's rules for trial termination, the probability of observing five consecutive lack of responses was 0.03 for an estimated 50% ORR (Gehan, 1961). Thus, as a first step, five patients were included. In case of no objective response, the trial would have been stopped. In the case of at least one objective response, the trial would be continued.
Statistical methods
All patients were included into the analysis. Data were presented as median and extremes. The Wilcoxon test was performed to compare the plasma DHA level at the end of the loading period with baseline. The relationship between patient DHA incorporation and baseline characteristics or toxicities observed was analysed using the Mann–Whitney test or Fisher's exact test. The Kaplan–Meier method and log-rank test were applied for survival calculation. Statistical analyses were performed with the GraphPad Prism 4 software (GraphPad Software, Inc., San Diego, USA). P< 0.05 was regarded as significant.
Results
Patients were enrolled between February 2001 and April 2003 to receive the DHA/FEC combination. Table 1 presents patients’ characteristics at baseline. The median age was 58 years, performance status was 0 or 1 in 96% of cases. Most patients (19 out of 25) had received earlier therapy, including adjuvant or neo-adjuvant anthracycline-based chemotherapy (40%), chest wall radiation therapy or hormonal therapy (adjuvant or metastatic) (64%). Twelve patients had received tamoxifene as an adjuvant hormonal therapy (two patients had been switched to an aromatase inhibitor). The median duration of this hormonal treatment was 29 months (range 8–60 months), one patient had received hormonal therapy for 5 years. Four patients had received hormonal therapy as first-line treatment for metastases. Disease extension was severe in most cases, with 72% of liver metastases. Forty per cent had three or more metastatic sites.
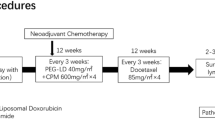
The median DHA level at baseline was 2.6% of total fatty acids (range 1.6% to 5%). At the end of the loading period, it reached 5.1% (range 2.5% to 8.3%, P<0.0001) (Figure 1A). The DHA level was 6.0% at cycle 4 (range 2.9% to 9.7%) and 6.4% at cycle 6 (range 3.5% to 8.9%). The extent of DHA increase at the end of the loading period differed among patients. It ranged from 0% to 4.3% with a Gaussian distribution (Figure 1B), allowing the definition of two groups of patients according to their ability to incorporate DHA: a group with high-DHA (H-DHA) incorporation and a group with lower-DHA incorporation (L-DHA), the cutoff being the median value (2.5%). Baseline characteristics of the two groups were balanced: median age was 58 years in the H-DHA group and 57 years in the L-DHA group, 58% of patients had a performance status of 1 in the H-DHA group vs 62% in the L-DHA group, one patient had a performance status of 2 in the L-DHA group, 83% of patients had 2 or more metastatic locations in the H-DHA group vs 77% in the L-DHA group and there was liver involvement in 67% and 77% of cases, respectively. Oestrogen receptors in primary tumour were positive in 67% or 69% of patients in the H-DHA or L-DHA groups, respectively. One patient had a positive HER-2 status in the primary tumour in the H-DHA group vs two patients in the L-DHA group. The median metastases-free interval was 3 years in both groups (range 0–13 years in the H-DHA group and 0–20 years in the L-DHA group). Five patients had synchronous metastases at the time of cancer diagnosis in the H-DHA group and two patients in the L-DHA group (P=0.2, Fisher's test). Three patients received adjuvant hormonal therapy by tamoxifene in the H-DHA group and nine patients in the L-DHA group (P=0.05, Fisher's test). Tamoxifene was switched to an aromatase inhibitor in two patients in the L-DHA group (none in the H-DHA group). The baseline DHA level was 2.6% (range 1.6–4.3%) in the H-DHA group and 2.7% (range 1.8–5%) in the L-DHA group.
Differential incorporation of DHA among patients. (A) DHA increase after the loading period (LP). Metastatic breast cancer patients received 1.8 g/day of oral DHA at inclusion. DHA plasma phospholipid level was measured at baseline and before initiation of chemotherapy. DHA increase was significant (P<0.0001, Wilcoxon test). (B) Patient distribution according to the extent of DHA increase. The median of this distribution (2.5%) was used as a threshold to define two groups of patients with a high- (H-DHA, grey bars) or low- (L-DHA, white bars) DHA increase. Black (▴) or open (△) triangles stand for H-DHA or L-DHA incorporation.
Efficacy
Among the first five patients evaluable for response, we observed two PRs; therefore, the trial was completed. All patients took the DHA supplementation as planned, with a global compliance of 90%. A total of 163 cycles of FEC were administered along with DHA supplementation, with a median number of six cycles per patient (range 3–9) in H-DHA or L-DHA incorporation groups.
The ORR was 44% (95% CI, 24.5–63.5) (1 CR and 10 PR). There were 11 SD cases and three PD cases. The clinical benefit achieved was 88%. With a mean follow-up of 31 months (range 2–96 months), the median TTP was 6 months (95% CI, 2.8–8.7 months) (Figure 2A). Median OS was 22 months (95% CI, 17–33 months) (Figure 2C). One patient was still living as of June 2009. TTP (Figure 2B) was greater in the H-DHA group, with a median TTP of 8.7 months vs 3.5 months in the L-DHA group (P=0.02). OS (Figure 2D) was significantly greater in the H-DHA group with a median survival time of 34 months vs 18 months in the L-DHA group (P=0.007). The type of post-trial treatments did not differ between the two groups. Two patients received no further systemic treatment (one in each group), 15 patients received an aromatase inhibitor (6 out of 12 and 9 out of 13 in the H-DHA and L-DHA groups, respectively, ns) and 7 patients received chemotherapy by docetaxel (4 out of 12 and 3 out of 13 in the H-DHA and L-DHA groups, respectively, ns). The median number of lines of post-trial chemotherapy and anti-cancer drugs used (including a taxane or trastuzumab) was similar in both groups. Survival analysis by hormonal status or by adjuvant hormonal therapy (received or not) showed no influence of these factors on survival (data not shown).
Survival curves. Global population TTP (A) or OS (C) is indicated with a mean follow-up of 31 months (2–96 months). This population was divided into two groups as described in the legend of Figure 1. TTP (B) or OS (D) by DHA incorporation was significantly different for patients with H-DHA (▪) or L-DHA (▾) incorporation (log-rank test).
Safety
All patients were evaluated for safety. DHA supplementation was well tolerated. No DHA-related adverse events were observed either during the loading period or FEC chemotherapy. Delay in the administration of chemotherapy occurred in 15% of cycles and was lower than 8 days in 84% of cases. Reduction of epirubicin dose occurred only once (0.6% of cycles). Principal grade 3 or 4 toxicity was neutropaenia (80%), with one case of febrile aplasia. Anaemia and thrombopaenia occurred in 8% of cases (2 out of 25 patients). Complete alopaecia occurred in 80% of cases. No grade 4 non-haematological adverse events were recorded. Grade 3 toxicity was infrequent. No grade 3 or 4 cardiac toxicity was reported. Sonographic measurement of cardiac function identified a non-symptomatic decrease of the LVEF in three patients (grade 1 in two cases and grade 2 in one case). According to DHA incorporation, patients in the H-DHA group experienced anaemia and thrombopaenia less frequently (P=0.01) as compared with those in the L-DHA group (Table 2). Non-haematological toxicities did not differ among groups.
Treatment was discontinued as a consequence of completion of therapy in 21 patients, early disease progression in one patient, haematological toxicity in one patient and non-symptomatic decrease in LVEF (to a value of 45%) in one patient. One patient died 15 days after the administration of the third cycle of chemotherapy. This patient was 71 years old and had a sudden alteration of consciousness leading to rapid death. The precise cause of death could not be identified, but the occurrence of stroke was suspected. The evaluation made after two cycles did not indicate any tumour progression. This serious adverse event was not considered to be related to treatment.
Discussion
This trial is a logical extension of earlier studies carried out in rodents and shows that a defined food component, namely DHA, can turn malignant mammary tumours from resistant to sensitive to chemo- (Colas et al, 2006) or radiation therapy (Colas et al, 2004). Our data show for the first time that a dietary intervention targeted on DHA is a feasible approach that has potential to substantially increase survival in metastatic breast cancer patients treated with chemotherapy.
When compared with historical data, the ORR observed in our population was within the range (30% to 60%) of that which has been reported in frontline FEC 75 chemotherapy for breast cancer metastasis (FESG, 1991, 2000; Pavesi et al, 1995; Pacini et al, 2000; Capotorto et al, 2003; Bonneterre et al, 2004). In terms of survival, frontline FEC 75 chemotherapy in this setting has been found to induce a median TTP ranging from 6 to 13 months and a median OS ranging from 18 to 23 months, with one single study reporting 28 months (FESG, 1991, 2000; Pavesi et al, 1995; Pacini et al, 2000; Capotorto et al, 2003; Bonneterre et al, 2004). Although the median TTP (6 months) and OS (22 months) in our study were within the frame of published data, it should be stressed that our patient population had a particularly poor prognosis, as 68% had liver metastases in addition to other sites of metastases. The median OS of patients having liver metastases was reported to be 14 months (Atalay et al, 2003). Moreover, we observed wide disparities in survival among patients, ranging from 2.8 to 8.7 months for TTP and from 17 to 33 months for OS (95% CI).
Orally provided fatty acids must be incorporated in cell membranes to be effective, and this could be impeded in various individual cancer patients by a variety of metabolic defects. For these reasons, this study has been analysed as a function of DHA incorporation. We observed wide inter-individual disparities in DHA incorporation in plasma phospholipids at the end of the loading period. Those disparities were unexpected, as global compliance was 90% of the planned dose. We identified that survival was associated with the extent of DHA incorporated into plasma phospholipids. When patients were stratified according to this factor, TTP was significantly higher in patients with an H-DHA incorporation (8.7 months vs 3.5 months in patients with L-DHA incorporation), suggesting a greater efficacy of chemotherapy. Most importantly, OS was almost doubled in patients with H-DHA incorporation (34 months vs 18 months). The significant difference observed between patients with H-DHA or L-DHA incorporation could not be ascribed to differences in earlier hormonal therapy, time to metastases, DHA level at baseline or post-trial treatments among the two patient groups. Although the design of the study does not allow for confirmation that DHA increased the basal activity of chemotherapy, the fact that both TTP and OS were vastly different according to the level of DHA incorporated indicates that the addition of DHA to chemotherapy had a beneficial effect when highly incorporated. This assumption was strengthened by the fact that no factor other than DHA incorporation could account for the difference in survival observed. In particular, the level of any contaminants with endocrine disruptor activity in DHASCO capsules was too low (under the pg/day) to account for a bias in this population of patients consisting of 68% ER positives.
DHA is a ubiquitous structural component of cell membranes. DHA is mainly provided by diet, as its rate of endogenous synthesis through elongation and desaturation steps from α-linolenic acid is limited (Burdge, 2006). In tumour tissues, DHA is thought to originate from diet, because a positive correlation between the DHA content of tumour and non-tumour epithelial breast tissues has been observed, and because the fatty acid desaturation activity in human breast tumour tissues has been found to be very low or absent (Chajes et al, 1995). After absorption, DHA incorporates into plasma phospholipids, which is a route for the delivery of DHA to tissues (Lagarde et al, 2001; Polozova et al, 2006). This includes tumours, as indicated by the concomitant increase in the DHA content of plasma phospholipids and tumours in cancer patients reported by Senkal et al (2005). Thus, besides its relevance as a biomarker of DHA intake, plasma phospholipid DHA content may also reflect the availability of DHA to tissues, including tumours. Therefore, the disparities in DHA incorporation into plasma phospholipids could be an indicator of a differential incorporation of DHA into metastatic tumour tissue among patients, which is higher in patients with a marked plasma DHA increase. Our results indicate that DHA incorporation is a relevant factor involved in chemotherapy efficacy. Therefore, during dietary interventions with DHA, appropriate conditions leading to a consistently elevated plasma DHA content in all patients have to be investigated. In hypotheses, the concomitance of DHA intake to food intake may influence DHA incorporation and has to be taken into account.
Interestingly, and compared with literature, we did not observe additional toxicity in normal tissues, including in patients with an H-DHA incorporation. Although DHA is a non-toxic compound (Kroes et al, 2003), its incorporation into blood cell precursors (Vidgren et al, 1997) theoretically could have resulted in an increased myelosuppression during its prolonged association (16 to 22 weeks) with FEC chemotherapy. However, no increased haematological toxicity was found as compared with historical data. It is worth stressing that the reported rates of haematological toxicity rely heavily on the frequency of blood count assessment. They could range from 7% to 84% for neutropaenia, 1% to 21% for anaemia or from 1% to 9% for thrombocytopaenia (Stewart et al, 1997; Blajman et al, 1999; FESG, 2000; Pacini et al, 2000; Bonneterre et al, 2004; Zielinski et al, 2005). A slightly lower toxicity of chemotherapy with respect to anaemia and thrombopaenia was even observed in the H-DHA group. This is in line with the protective effects of DHA against the gastrointestinal toxicity of chemotherapy or radiation therapy in experimental models (Hardman et al, 1999; Kato et al, 2002; Wen et al, 2003; Xue et al, 2007) or in patients (Minami et al, 2008).
As anthracycline-related myocardial toxicity has been considered as a consequence of direct myocardial injury by ROS generated by chemotherapy (Singal et al, 2000; Minotti et al, 2004), the addition of DHA could have potentially amplified this toxicity. However, no severe cardiac toxicity was reported in this trial. The lack of additional cardiac toxicity may result from an efficient ROS detoxification system by cardiomyocytes, although the possibility that ROS generation might not be the main determinant in anthracycline-related heart damage has already been considered in several studies (Olson et al, 1988; Minotti et al, 2004). Patients with an H-DHA incorporation did not show increased toxicities to FEC chemotherapy as compared with patients with an L-DHA incorporation. Taken together, our results suggest that DHA had a chemosensitising effect on metastases and not on non-tumour tissues, and, therefore, acted as a tumour-specific chemosensitiser. We are currently investigating potential mechanisms in vitro that may account for a differential effect of DHA on tissues. Recent data suggest that the anti-oxidant system of tumour cells may be altered during cancer progression, making tumour cells more sensitive to ROS damage (Mahéo et al, 2005; Vibet et al, 2008; Sun et al, 2009).
Our study has a number of strengths. It involves a homogeneous population of patients, all receiving identical treatment in one single cancer centre and being evaluated by one single medical team within a short period of inclusion. Although the number of patients involved in the study was small, survival as an end point and the length of follow-up give strength to the conclusion, as time to death was not censored in 96% of the patients. This study also has several limitations. It does not allow for a definitive assessment of the efficacy of DHA combination to chemotherapy. The design was not dedicated to comparing two sub-populations according to their level of plasma DHA. However, the difference in the likelihood of survival between the two populations suggests that DHA has a potential to increase the activity of chemotherapy, and that this potential may be proportional to its degree of incorporation. We are fully aware that the association reported between DHA incorporation into plasma phospholipids and metastatic cancer outcome subsequent to chemotherapy does not ensure a causality relationship. These results warrant confirmation through a larger placebo-controlled randomised phase III clinical trial stratified on patients’ DHA incorporation.
In conclusion, this study shows that addition of DHA to chemotherapy is devoid of adverse side effects and might improve the outcome of metastatic breast cancer patients. These results suggest that DHA has a potential to specifically chemosensitise tumours. This study represents the incentive to set up a prospective-controlled randomised trial aimed at identifying the place of dietary DHA in breast cancer treatments.
References
Arterburn LM, Hall EB, Oken H (2006) Distribution, interconversion, and dose response of n-3 fatty acids in humans. Am J Clin Nutr 83: 1467–1476
Atalay G, Biganzoli L, Renard F, Paridaens R, Cufer T, Coleman R, Calvert AH, Gamucci T, Minisini A, Therasse P, Piccart MJ, EORTC Breast Cancer and Early Clinical Studies Groups (2003) Clinical outcome of breast cancer patients with liver metastases alone in the anthracycline-taxane era: a retrospective analysis of two prospective, randomised metastatic breast cancer trials. Eur J Cancer 39: 2439–2449
Begin ME, Ells G, Das UN, Horrobin DF (1986) Differential killing of human carcinoma cells supplemented with n-3 and n-6 polyunsaturated fatty acids. J Natl Cancer Inst 77: 1053–1062
Blajman C, Balbiani L, Block J, Coppola F, Chacon R, Fein L, Bonicatto S, Alvarez A, Schmilovich A, Delgado FM (1999) A prospective, randomized Phase III trial comparing combination chemotherapy with cyclophosphamide, doxorubicin, and 5-fluorouracil with vinorelbine plus doxorubicin in the treatment of advanced breast carcinoma. Cancer 85: 1091–1097
Bonneterre J, Dieras V, Tubiana-Hulin M, Bougnoux P, Bonneterre ME, Delozier T, Mayer F, Culine S, Dohoulou N, Bendahmane B (2004) Phase II multicentre randomised study of docetaxel plus epirubicin vs 5-fluorouracil plus epirubicin and cyclophosphamide in metastatic breast cancer. Br J Cancer 91: 1466–1471
Burdge GC (2006) Metabolism of alpha-linolenic acid in humans. Prostaglandins Leukot Essent Fatty Acids 75: 161–168
Capotorto AM, Pavesi L, Pedrazzoli P, Da Prada GA, Zamagni C, Massidda B, Farris A, Martoni A, Lelli G, Robustelli della Cuna G (2003) Randomized, controlled, multicenter phase III trial of standard-dose fluorouracil-epirubicin-cyclophosphamide (FEC), compared with time-intensive FEC (FEC-G) and mitoxantrone-methotrexate-mitomycin C (MMM-G) in metastatic breast carcinoma. J Chemother 15: 184–191
Chajès V, Hultén K, Van Kappel AL, Winkvist A, Kaaks R, Hallmans G, Lenner P, Riboli E (1999) Fatty-acid composition in serum phospholipids and risk of breast cancer: an incident case-control study in Sweden. Int J Cancer 83: 585–590
Chajes V, Lanson M, Fetissof F, Lhuillery C, Bougnoux P (1995) Membrane fatty acids of breast carcinoma: contribution of host fatty acids and tumor properties. Int J Cancer 63: 169–175
Colas S, Germain E, Arab K, Maheo K, Goupille C, Bougnoux P (2005) Alpha-tocopherol suppresses mammary tumor sensitivity to anthracyclines in fish oil-fed rats. Nutr Cancer 51: 178–183
Colas S, Mahéo K, Denis F, Goupille C, Hoinard C, Champeroux P, Tranquart F, Bougnoux P (2006) Sensitization by dietary docosahexaenoic acid of rat mammary carcinoma to anthracycline: a role for tumor vascularization. Clin Cancer Res 12: 5879–5886
Colas S, Paon L, Denis F, Prat M, Louisot P, Hoinard C, Le Floch O, Ogilvie G, Bougnoux P (2004) Enhanced radiosensitivity of rat autochthonous mammary tumors by dietary docosahexaenoic acid. Int J Cancer 109: 449–454
Folch J, Lees M, Sloane Stanley GH (1957) A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem 226: 497–509
French Epirubicin Study Group (1991) A prospective randomized trial comparing epirubicin monochemotherapy to two fluorouracil, cyclophosphamide, and epirubicin regimens differing in epirubicin dose in advanced breast cancer patients. J Clin Oncol 9: 305–312
French Epirubicin Study Group (2000) Epirubicin-based chemotherapy in metastatic breast cancer patients: role of dose-intensity and duration of treatment. J Clin Oncol 18: 3115–3124
Gehan EA (1961) The determination of the number of patients required in a preliminary and a follow-up trial of a new chemotherapeutic agent. J Chronic Dis 13: 346–353
Germain E, Bonnet P, Aubourg L, Grangeponte MC, Chajes V, Bougnoux P (2003) Anthracycline-induced cardiac toxicity is not increased by supplementation omega-3 fatty acids. Pharmacol Res 47: 111–117
Germain E, Chajes V, Cognault S, Lhuillery C, Bougnoux P (1998) Enhancement of doxorubicin cytotoxicity by polyunsaturated fatty acids in the human breast tumor cell line MDA-MB-231: relationship to lipid peroxidation. Int J Cancer 75: 578–583
Hardman WE, Avula CP, Fernandes G, Cameron IL (2001) Three percent dietary fish oil concentrate increased efficacy of doxorubicin against MDA-MB 231 breast cancer xenografts. Clin Cancer Res 7: 2041–2049
Hardman WE, Moyer MP, Cameron IL (1999) Fish oil supplementation enhanced CPT-11 (irinotecan) efficacy against MCF7 breast carcinoma xenografts and ameliorated intestinal side-effects. Br J Cancer 81: 440–448
Kato T, Hancock RL, Mohammadpour H, McGregor B, Manalo P, Khaiboullina S, Hall MR, Pardini L, Pardini RS (2002) Influence of omega-3 fatty acids on the growth of human colon carcinoma in nude mice. Cancer Lett 187: 169–177
Kroes R, Schaefer EJ, Squire RA, Williams GM (2003) A review of the safety of DHA45-oil. Food Chem Toxicol 41: 1433–1446
Lagarde M, Bernoud N, Brossard N, Lemaitre-Delaunay D, Thiès F, Croset M, Lecerf J (2001) Lysophosphatidylcholine as a preferred carrier form of docosahexaenoic acid to the brain. J Mol Neurosci 16: 201–204
Mahéo K, Vibet S, Steghens JP, Dartigeas C, Lehman M, Bougnoux P, Goré J (2005) Differential sensitization of cancer cells to doxorubicin by DHA: a role for lipoperoxidation. Free Radic Biol Med 39: 742–751
Menendez JA, Lupu R, Colomer R (2005) Exogenous supplementation with omega-3 polyunsaturated fatty acid docosahexaenoic acid (DHA; 22:6n-3) synergistically enhances taxane cytotoxicity and downregulates Her-2/neu (c-erbB-2) oncogene expression in human breast cancer cells. Eur J Cancer Prev 14: 263–270
Minami Y, Miyata H, Doki Y, Yano M, Yamasaki M, Takiguchi S, Fujiwara Y, Yasuda T, Monden M (2008) Omega-3 fatty acid-containing diet (Racol) reduces toxicity of chemoradiation therapy for patients with esophageal cancer. Gan To Kagaku Ryoho 35: 437–440
Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L (2004) Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol Rev 56: 185–229
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5: 649–655
Olson RD, Mushlin PS, Brenner DE, Fleischer S, Cusack BJ, Chang BK, Boucek Jr RJ (1988) Doxorubicin cardiotoxicity may be caused by its metabolite, doxorubicinol. Proc Natl Acad Sci USA 85: 3585–3589
Pacini P, Rinaldini M, Algeri R, Guarneri A, Tucci E, Barsanti G, Neri B, Bastiani P, Marzano S, Fallai C (2000) FEC (5-fluorouracil, epidoxorubicin and cyclophosphamide) versus EM (epidoxorubicin and mitomycin-C) with or without lonidamine as first-line treatment for advanced breast cancer. A multicentric randomised study. Final results. Eur J Cancer 36: 966–975
Pavesi L, Preti P, Da Prada G, Pedrazzoli P, Poggi G, Robustelli della Cuna G (1995) Epirubicin versus mitoxantrone in combination chemotherapy for metastatic breast cancer. Anticancer Res 15: 495–501
Polozova A, Gionfriddo E, Salem Jr N (2006) Effect of docosahexaenoic acid on tissue targeting and metabolism of plasma lipoproteins. Prostaglandins Leukot Essent Fatty Acids 75: 183–190
Senkal M, Haaker R, Linseisen J, Wolfram G, Homann HH, Stehle P (2005) Preoperative oral supplementation with long-chain Omega-3 fatty acids beneficially alters phospholipid fatty acid patterns in liver, gut mucosa, and tumor tissue. JPEN J Parenter Enteral Nutr 29: 236–240
Shao Y, Pardini L, Pardini RS (1997) Intervention of transplantable human mammary carcinoma MX-1 chemotherapy with dietary menhaden oil in athymic mice: increased therapeutic effects and decreased toxicity of cyclophosphamide. Nutr Cancer 28: 63–73
Singal PK, Li T, Kumar D, Danelisen I, Iliskovic N (2000) Adriamycin-induced heart failure: mechanism and modulation. Mol Cell Biochem 207: 77–85
Stewart DJ, Evans WK, Shepherd FA (1997) Cyclophosphamide and fluorouracil combined with mitroxantrone vs doxorubicin for breast cancer: superiority of doxorubicin. J Clin Oncol 15: 1897–1905
Sun W, Kalen AL, Smith BJ, Cullen JJ, Oberley LW (2009) Enhancing the antitumor Activity of Adriamycin and Ionizing radiation. Cancer Res 69: 4294–4300
Vibet S, Goupille C, Bougnoux P, Steghens JP, Goré J, Mahéo K (2008) Sensitization by docosahexaenoic acid (DHA) of breast cancer cells to anthracyclines through loss of glutathione peroxidase (GP × 1) response. Free Radic Biol Med 44: 1483–1491
Vidgren HM, Agren JJ, Schwab U, Rissanen T, Hanninen O, Uusitupa MI (1997) Incorporation of n-3 fatty acids into plasma lipid fractions, and erythrocyte membranes and platelets during supplementation supplementation with fish, fish oil, and docosahexaenoic acid-rich oil among healthy young men. Lipids 32: 697–705
Wang Z, Butt K, Wang L, Liu H (2007) The effect of seal oil on paclitaxel induced cytotoxicity and apoptosis in breast carcinoma MCF-7 and MDA-MB-231 cell lines. Nutr Cancer 58: 230–238
Wen B, Deutsch E, Opolon P, Auperin A, Frascogna V, Connault E, Bourhis J (2003) N-3 polyunsaturated fatty acids decrease mucosal/epidermal reactions and enhance antitumour effect of ionising radiation with inhibition of tumour angiogenesis. Br J Cancer 89: 1102–1107
Xue H, Sawyer MB, Field CJ, Dieleman LA, Baracos VE (2007) Nutritional modulation of antitumor efficacy and diarrhea toxicity related to irinotecan chemotherapy in rats bearing the ward colon tumor. Clin Cancer Res 13: 7146–7154
Zielinski C, Beslija S, Mrsic-Krmpotic Z, Welnicka-Jaskiewicz M, Wiltschke C, Kahan Z, Grgic M, Tzekova V, Inbar M, Cervek J, Chernozemsky I, Szanto J, Spanik SM, Ghilezan N, Pawlega J, Vrbanec D, Khamtsov D, Soldatenkova V, Brodowicz T (2005) Gemcitabine, epirubicin, and paclitaxel vs fluorouracil, epirubicin, and cyclophosphamide as first-line chemotherapy in metastatic breast cancer: a Central European Cooperative Oncology Group International, multicenter, prospective, randomized phase III trial. J Clin Oncol 23: 1401–1408
Acknowledgements
We thank MB Orgerie, A Reynaud-Bougnoux, S Chapet, L Alcaraz, A Veret and F Denis for their involvement in patient's enrolment and follow-up; ML Jourdan for blood sample collection and J Leguarrec, M Pinault, MA Baucher and C Goupille for fatty acid analysis. This study was supported by grants from the French Ministry of Health (PHRC), INSERM, the Tours University Hospital and University François Rabelais and the section of Indre-et-Loire of the French League Against Cancer. DHASCO (DHA Single Cell Oil, which is a registered trademark of Martek Biosciences Corp., Columbia MD, USA) capsules were graciously provided by Martek Biosciences Corp. (Columbia MD, USA).
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bougnoux, P., Hajjaji, N., Ferrasson, M. et al. Improving outcome of chemotherapy of metastatic breast cancer by docosahexaenoic acid: a phase II trial. Br J Cancer 101, 1978–1985 (2009). https://doi.org/10.1038/sj.bjc.6605441
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605441
Keywords
This article is cited by
-
Lipid-lowering drugs and cancer: an updated perspective
Pharmacological Reports (2024)
-
Anti-inflammatory effect of combining fish oil and evening primrose oil supplementation on breast cancer patients undergoing chemotherapy: a randomized placebo-controlled trial
Scientific Reports (2023)
-
Adjunction of a fish oil emulsion to cytarabine and daunorubicin induction chemotherapy in high-risk AML
Scientific Reports (2022)
-
Pharmaceutical nanoformulation strategies to spatiotemporally manipulate oxidative stress for improving cancer therapies — exemplified by polyunsaturated fatty acids and other ROS-modulating agents
Drug Delivery and Translational Research (2022)
-
Oxidative stress and inflammation: determinants of anthracycline cardiotoxicity and possible therapeutic targets
Heart Failure Reviews (2021)