Revised: November 28, 2008
Accepted: December 5, 2008
Published online: January 7, 2009
In addition to regulating acid secretion, the gastric antral hormone gastrin regulates several important cellular processes in the gastric epithelium including proliferation, apoptosis, migration, invasion, tissue remodelling and angiogenesis. Elevated serum concentrations of this hormone are caused by many conditions, particularly hypochlorhydria (as a result of autoimmune or Helicobacter pylori (H pylori)-induced chronic atrophic gastritis or acid suppressing drugs) and gastrin producing tumors (gastrinomas). There is now accumulating evidence that altered local and plasma concentrations of gastrin may play a role during the development of various gastric tumors. In the absence of H pylori infection, marked hypergastrinemia frequently results in the development of gastric enterochromaffin cell-like neuroendocrine tumors and surgery to remove the cause of hypergastrinemia may lead to tumor resolution in this condition. In animal models such as transgenic INS-GAS mice, hypergastrinemia has also been shown to act as a cofactor with Helicobacter infection during gastric adenocarcinoma development. However, it is currently unclear as to what extent gastrin also modulates human gastric adenocarcinoma development. Therapeutic approaches targeting hypergastrinemia, such as immunization with G17DT, have been evaluated for the treatment of gastric adenocarcinoma, with some promising results. Although the mild hypergastrinemia associated with proton pump inhibitor drug use has been shown to cause ECL-cell hyperplasia and to increase H pylori-induced gastric atrophy, there is currently no convincing evidence that this class of agents contributes towards the development of gastric neuroendocrine tumors or gastric adenocarcinomas in human subjects.
- Citation: Burkitt MD, Varro A, Pritchard DM. Importance of gastrin in the pathogenesis and treatment of gastric tumors. World J Gastroenterol 2009; 15(1): 1-16
- URL: https://www.wjgnet.com/1007-9327/full/v15/i1/1.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.1
Gastric epithelial malignancy represents a significant burden of disease. The commonest lesion is gastric adenocarcinoma, which is the fourth commonest malignancy worldwide, and because it is associated with a high mortality, this tumor remains the second commonest cause of cancer-related death globally. The distribution of gastric epithelial malignancies is not uniform between different populations, with increased prevalence being found in East Asia including Japan and China (where 42% of cases occur), as well as in Eastern Europe and South America[1]. This epidemiology raises significant questions as to the predisposing factors for gastric malignancy. Current data suggest that a number of different variables affect an individual’s risk of gastric carcinogenesis, amongst which are environmental factors such as infection with Helicobacter pylori (H pylori), smoking and diet, as well as host factors such as achlorhydria and specific cytokine polymorphisms. Another important host factor which may play a role during gastric carcinogenesis is the hormone gastrin.
As well as acting as a potential cofactor during gastric adenocarcinoma development, gastrin is also known to play a major role in the pathogenesis of other gastric tumor types, particularly neuroendocrine (carcinoid) tumors. There is therefore accumulating evidence that gastrin not only influences tumor development, but could also be a potential therapeutic target for various gastric neoplasias. These issues will be the main focus of this editorial.
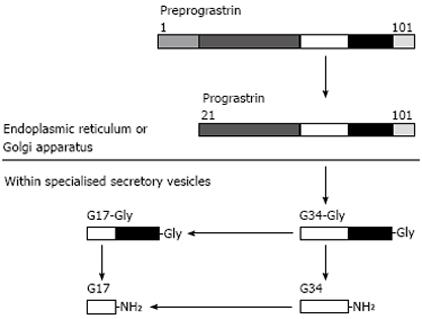
The presence of a hormone that stimulated gastric acid secretion in the pyloric mucosa was first demonstrated in 1906[2]. Gastrin was subsequently shown to be secreted from neuroendocrine G cells which are principally located in the antrum of the stomach. The gastrin gene is located on the long arm of chromosome 17 and encodes a 101 amino acid polypeptide, preprogastrin. This gene product is subjected to a series of post translational modifications which result in the synthesis of a number of biologically active peptides[3] (Figure 1). Immediately after translation, preprogastrin is cleaved to form progastrin, which is transported to the Golgi network, where it is packaged into secretory vesicles. Further post-translational modification occurs at this site, firstly to form gastrin-34-Gly, the C-terminal glycine extended form of gastrin-34. This peptide may then undergo further cleavage into gastrin-17-Gly or amidation to generate gastrin-34, which in turn may be cleaved to form gastrin-17. Progastrin, glycine extended gastrins and amidated gastrins are all biologically active and exert different functions within gastric and other mucosae. Progastrin and glycine extended gastrins act particularly on the colonic mucosa as mitogens[45], glycine extended and amidated gastrins have been shown to affect the differentiation of gastric oxyntic mucosa, whilst amidated gastrin promotes cell proliferation as well as acid secretion in the stomach. In the human stomach, the conditions for post-translational modification of gastrin are such that there is almost complete amidation of glycine extended forms of gastrin, hence the predominant form of secreted gastrin is gastrin-17[3].
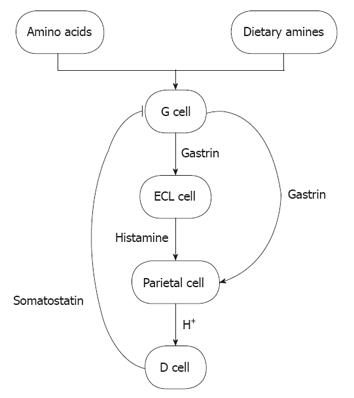
Acid secretion: Gastrin is secreted in response to a number of luminal stimuli, including the presence of amino acids and dietary amines (reviewed in[3]). Calcium receptors on the surface of the G-cell also sense luminal calcium and modulate the gastrin secretory response[6], with increased calcium resulting in increased gastrin secretion. Following secretion into the gastric vasculature, gastrin binds to CCK-2 receptors, which are expressed on the surface of gastric enterochromaffin-like (ECL) cells and parietal cells[7] (Figure 2). The predominant mode of secretagogue action is via ECL cell secretion of histamine and this pathway effectively amplifies the prosecretory signal. Continued gastrin secretion is negatively regulated by the secretion of somatostatin via D-cells, which are located in the oxyntic mucosa. In physiological states, these mechanisms maintain appropriate gastric pH.
Proliferation: Studies in dogs in 1972 provided the first evidence of mucosal proliferation in response to gastrin[8], however these studies were triggered by earlier clinical observations of increased gastric mucosal proliferation in patients with Zollinger-Ellison syndrome (ZES). Subsequently, increased fundic mucosal proliferation was demonstrated in rodent models including Mastomys following the administration of an H2 receptor antagonist which rendered them hypergastrinemic. These animals demonstrated gastric gland elongation and increased numbers of cells which stained for Ki67, a marker of proliferation[9]. In normal humans, the infusion of gastrin at supraphysiological levels has also been shown to result in increased gastric cell proliferation, as demonstrated by 3H-thymidine labelling studies[10].
Endocrine cell proliferation in the stomachs of patients with ZES was first reported in 1974[11]. Further evidence that hypergastrinemia provides a proliferative drive to ECL cells emerged from studies in which rats were rendered hypergastrinemic by treatment with either proton pump inhibitor (PPI) or H2 receptor antagonist drugs. ECL cell hyperplasia was not observed in control untreated animals or in rats that had been antrectomized prior to treatment with high-dose PPI[12]. These observations in rats have to some extent been corroborated in other species, as ECL cell hyperplasia has now also been demonstrated following PPI treatment of chickens, hamsters and guinea pigs[1314]. ECL cell hyperplasia of this magnitude does not however appear to occur in mice or humans treated with acid suppressant drugs.
To investigate the molecular mechanisms by which gastrin promotes proliferation, a number of gastric cancer cell lines that express the CCK-2 receptor have been employed. It has recently been shown that the proliferation of MKN-45 cells, which are derived from a poorly differentiated gastric carcinoma and which have been reported to express the CCK-2 receptor, decreased when treated with the CCK-2 receptor antagonist AG-041R[15]. Several cell lines which have independently been stably transfected with the CCK-2 receptor (but using different expression vectors) have been generated from AGS gastric cancer cells (which do not constitutively express the CCK-2 receptor). The AGS-B cell line (transfected with human full-length CCK-2 receptor using the pcDNA I vector and neomycin selection) was found to proliferate more rapidly in the presence of gastrin, a process that was associated with the upregulation of cyclin D1[16]. In contrast, the effects of gastrin on the proliferation of AGS-GR cells (transfected with the human full length CCK-2 receptor driven by the EF1αpromoter under puromycin selection) were more complex. When cultured in the presence of gastrin-17, AGS-GR cells showed a reduced rate of proliferation, an effect that was abrogated by the addition of a CCK-2 receptor antagonist. However, when AGS-GR cells were co-cultured with AGS cells that had been transfected with a green fluorescent protein producing construct (AGS-GFP cells) in the presence of serum-free medium, gastrin exposure caused an increase in the proliferation of the AGS-GFP cells. This suggests that gastrin treatment of AGS-GR cells results in the secretion of growth factors that are capable of acting in a paracrine manner to stimulate the proliferation of AGS-GFP cells. Further analysis of the underlying mechanisms showed that epidermal growth factor ligands, particularly heparin binding epidermal growth factor (HB-EGF) were involved[17].
HB-EGF promotes cell cycling and is overexpressed by a number of cancer cell lines, including some gastric cancer cell lines and is of particular relevance to this article as it provides a potential molecular link between H pylori infection, gastrin and increased cell proliferation[18]. H pylori infection of gastric cancer cell lines has been shown to significantly increase HB-EGF levels and this effect is dependent upon the presence of the CCK-2 receptor. The most likely explanation is that H pylori induces cells to secrete gastrin, which in turn binds to and activates the CCK-2 receptor, resulting in HB-EGF secretion. This hypothesis is supported by evidence from animal models, as INS-GAS hypergastrinemic mice also overexpress HB-EGF in the premalignant lesions which develop following Helicobacter felis (H felis) infection[19]. This may partly explain the observed synergy between hypergastrinemia and Helicobacter infection during gastric carcinogenesis in this animal model.
Apoptosis: Apoptosis is a fundamental cellular process which is often dysregulated during the development of malignancy. There is accumulating evidence that gastrin modulates the apoptosis of both normal and transformed gastric epithelial cells and these mechanisms may contribute towards tumor development.
Several models of carcinogenesis are based upon the somatic mutation hypothesis proposed by Vogelstein in relation to colon cancer[20]. This hypothesis suggests that sequential defects are acquired by a tissue stem cell, eventually leading to the development of dysplastic and malignant phenotypes. This hypothesis suggests that an early failure in targeting mutated stem cells for apoptosis allows them to survive and generate mutated clones which progress to cancer. In the stomach however, an alternative mechanism of adenocarcinoma development has recently been proposed, as the gastric cancers which arise in H felis infected mice appear to develop in tissue that was originally derived from bone marrow stem cells. Houghton, Wang and colleagues studied C57BL/6 mice which had undergone bone marrow transplantation from GFP producing mouse strains or ROSA26 mice, thus allowing tissues that originated from the bone marrow rather than preexisting mucosal stem cells to be observed[21]. Following H felis infection, gastric cancers developed in these mice at a similar rate to other H felis-infected C57BL/6 mice, however, the tumors arose in glands which produced GFP, indicating that the tissue was initially derived from the bone marrow transplant. The authors propose that gastric stem cells undergo apoptosis as a result of Helicobacter infection, and that the stem cell niche is replaced by pluripotent stem cells which were originally located in the bone marrow. These cells may be more susceptible to malignant transformation than the previously incumbent gastric epithelial stem cells.
Gastrin signalling via the CCK-2 receptor appears to increase the susceptibility of normal gastric epithelial cells in vivo to undergo apoptosis. In Mastomys treated with H2 antagonist drugs, a two-fold increase in apoptosis was observed in hypergastrinemic animals relative to controls[9]. In addition, when mice were subjected to 12 Gy gamma irradiation or Helicobacter infection, increased numbers of apoptotic cells were observed in the gastric corpus mucosa of hypergastrinemic animals[2223]. Increased radiation-induced apoptosis was demonstrated both in transgenic INS-GAS mice and also in a model of drug-induced hypergastrinemia involving FVB/N mice treated with omeprazole. Treatment with a CCK-2 receptor antagonist abolished the observed increases in gastric epithelial apoptosis in both cases, suggesting that this response is both gastrin and CCK-2 receptor dependent. In gastric biopsy samples obtained from humans with both H pylori infection and hypergastrinemia, similar observations of increased apoptosis were also made[23]. These results suggest that hypergastrinemia may increase the susceptibility of gastric epithelial stem cells to undergo apoptosis, thus permitting the engraftment of bone marrow derived cells as suggested by Houghton and Wang[21].
Antiapoptotic effects of gastrin have however also been described, particularly in transformed cell types. For example, amidated gastrin inhibits the apoptosis of rat pancreatic acinar cancer cells (AR42J), by signalling through a CCK-2 receptor and an AKT-mediated mechanism[2425]. Similarly, the human gastric cancer cell line MKN-45 has been shown to be more susceptible to apoptosis when treated with a CCK-2 receptor antagonist and this was associated with upregulation of Bax and downregulation of Bcl-2[15]. More recently, gastrin has also been shown to inhibit AGS-GR cell apoptosis in a manner dependent upon the expression of the anti-apoptotic protein mcl-1. Increased mcl-1 expression was also observed in the type 1 gastric neuroendocrine tumors of hypergastrinemic patients[26].
The effects of gastrin on gastric apoptosis therefore appear to depend upon the underlying physiological and pathological conditions. There are thus a number of important questions which still need to be answered, not only regarding the effects of gastrin on apoptosis in differing circumstances, but also regarding the role of apoptosis during the development of gastric carcinoma and other gastric malignancies.
Angiogenesis: Angiogenesis is an essential feature required for tumor survival. In a number of GI malignancies, cyclooxygenase (COX)-2, an important rate-limiting step in the prostaglandin synthesis pathway, has been implicated in enhancing angiogenesis. For example, in human studies, COX-2 expression has been associated with the development of a more dense microvasculature around gastric tumors[27]. Gastrin has been shown to enhance COX-2 secretion in AGS-E cells (which have been stably transfected with the full-length human CCK-2 receptor on a EF1αpromoter, but by a different research group from those who produced AGS-GR cells) via an Akt-dependent mechanism[28]. Studies of patients with atrophic gastritis secondary to chronic Helicobacter infection have shown that, in addition to elevated levels of gastrin, these patients also have significantly higher levels of COX-2 mRNA compared to unaffected controls, a phenomenon that is reversed after H pylori eradication[29]. The mechanisms mediating increased COX-2 transcription in this setting have not been fully investigated to date, and it is not clear whether this effect is solely related to hypergastrinemia associated with Helicobacter infection and gastric atrophy or whether additional independent factors also influence COX-2 production.
Case control studies of patients taking aspirin and other COX inhibiting drugs have demonstrated a reduction in relative risk not only of gastric cancer, but also of colon cancer. Aspirin now has an established role in colon cancer prevention, however, its role in preventing diseases of the gastric epithelium is less convincing, due in part to the increased risk of GI bleeding associated with its use. Selective COX-2 inhibitors may have some potential as gastric cancer chemopreventive agents, however the serious cardiovascular side effects associated with the long-term use of the current generation of these drugs makes it unlikely that they will be adopted for this purpose.
In addition to the potential indirect role of gastrin upon angiogenesis via COX-2 expression, gastrin has also been suggested to have direct effects upon angiogenesis using an in vitro system. When human umbilical vein endothelial cells (HUVECS) were seeded onto fibroblast monolayers, they formed vascular structures in response to various angiogenic stimuli, including both amidated and glycine extended forms of gastrin. This response was associated with increased production of HB-EGF and with elevated levels of matrix metalloproteinase (MMP)2, MMP3 and MMP9[30].
Migration and invasion: Other fundamental cellular processes which are involved in promoting carcinogenesis and that are modulated by hypergastrinemia are tissue remodeling and invasion. Gastric cancer development involves extensive remodeling of the gastric mucosa during a hypergastrinemic premalignant phase (atrophic gastritis), in order to institute the conditions required for gastric carcinogenesis. Similar mechanisms are thought to be responsible for the local invasion and metastasis that occur in frankly malignant lesions. These processes are complex and are controlled by numerous different mechanisms, however, gastrin does appear to play a regulatory role. For example, gastrin has been shown to increase levels of MMP-9 via an MAPK AP-1 dependent pathway in human patients with gastric cancers and gastric neuroendocrine tumors, resulting in tissue remodelling and invasion[31]. Serum levels of MMP-7 have also been found to be elevated in patients who were hypergastrinemic as a result of either MEN-1 or pernicious anemia, and similar observations have been made both in transgenic hypergastrinemic INS-GAS mice and in gastrin-knockout mice treated with exogenous gastrin[32].
AGS-GR cells have again been used to investigate the mechanisms responsible for the effects of gastrin upon cellular migration and invasion. In response to gastrin stimulation, AGS-GR cells undergo a morphological change, with the induction of a branched phenotype, coupled with extensive remodelling of the cell’s actin cytoskeleton. These effects were abrogated by treatment with a CCK-2 receptor antagonist and the alteration in morphology was not seen when the parent AGS cell line was exposed to gastrin. In addition to the morphological changes observed in this cell line, there was also evidence of a change in migration which was again mediated via a CCK-2 receptor-dependent pathway. AGS-GR cells, but not AGS cells showed increased migration when cultured in the presence of amidated gastrin and experiments involving the co-culture of AGS-GR and AGS-GFP cells demonstrated that the effects of gastrin on cell migration were at least in part due to paracrine signalling[33].
Generation of a number of transgenic mouse strains over the last 15 years has greatly facilitated understanding of the mechanisms by which members of the gastrin family of peptides regulate the processes involved in gastric epithelial carcinogenesis (summarised in Table 1).
| Transgenic strain | Transgenic abnormality | Gastric phenotype | Susceptibility to gastric carcinoma | Other relevant phenotype |
| hGAS[4] | Human gastrin minigene expressed in liver-resulting in elevated serum levels of human progastrin | No known gastric phenotype | Not altered | Increased colonic mucosal proliferation[4113] and susceptibility to azoxymethane-induced colon cancer[114] |
| MTI/G-Gly[5] | Human gastrin gene with two stop codons after glycine-72, spliced with MTI promoter. Transgenic animals have elevated serum levels of glycine extended gastrin | No known gastric phenotype | Not altered | Increased colonic mucosal proliferation[5] |
| INS-GAS[34] | Human gastrin minigene spliced with insulin promoter expressed in pancreatic islets-resulting in elevated serum levels of amidated gastrin | Initial gastric mucosal hypertrophy and excess gastric acid secretion. By 5 mo, gastric atrophy and hypochlorhydria. Increased gastric proliferation and increased susceptibility to apoptosis | Increased (spontaneous tumors at 20 mo and H Felis-induced tumors at 6 mo) | Increased colonic mucosalproliferation in proximal and distal colon but not rectum initially observed in 1-year-old animals[4], but no difference in apoptotic or mitotic rates seen in 10-12-wk-old mice[113] and no increase in AOM-induced cancers[114] |
| INS-GAS/ MTI/G-Gly[37] | MTI/G-Gly mice crossed with INS-Gas mice to result in a “double” transgenic mouse that expresses both increased amidated and glycine extended forms of gastrin | Hyperchlorhydric at birth but unlike INS-GAS, no mucosal atrophy at older ages. Reduced apoptosis compared to INS-GAS with similar levels of proliferation. Overall rates of malignant progression comparable to INS-GAS | Increased | |
| GAS-KO[38] | Gastrin knockout mice generated by targeted gene disruption | Achlorhydric with reduced parietal cell numbers (gastric atrophy), clustering of ECL cells at gland bases and increased TFF2-positive cells (spasmolytic polypeptide expressing metaplasia) | Increased | Increased susceptibility to azoxymethane-induced colon carcinogenesis[115] (despite normal untreated proliferation indices[113]) |
| CCK-B-null[49] | Gastrin receptor knockout mice generated by targeted gene disruption | Marked gastric atrophy and achlorhydria. Morphologically abnormal ECL cells with loss of normal secretory vesicles and replacement with dense core granules and microvesicles | Not reported | Increased sensitivity to dopamine[116] and altered behaviour in response to alcohol[117118] and other stimuli[119120] |
HGAS: hGas mice transgenically overexpress a complete human gastrin mini gene including the gastrin promoter region in some liver cells. Because the enzymes required for the post-translational processing of preprogastrin are not present in this tissue, hGas mice selectively overexpress human progastrin[4]. These mice show increased colonic proliferation and increased susceptibility to colonic carcinogenesis[4]. However, in contrast to the INS-GAS mice described below, there is no overt gastric phenotype, and no alterations were observed in gastric proliferation[4] or radiation-induced apoptosis[23] in comparison to wild-type. This suggests that the effects of the gastrin family of peptides on gastric mucosa are predominantly due to amidated forms of the hormone[4].
INS-GAS: In contrast to the liver, neuroendocrine cells, including those present in pancreatic islets, possess the appropriate enzymatic machinery to allow processing of progastrin into glycine extended and amidated forms of the hormone. Transgenic INS-GAS mice were created by expressing a human gastrin minigene spliced onto the insulin promoter and this resulted in expression of the gene in the pancreatic islets of adult animals. INS-GAS mice therefore have elevated serum concentrations of amidated gastrin[34]. At a young age, these mice have a two-fold increase in plasma gastrin levels compared to wild-type, show increased numbers of gastric parietal cells and ECL cells and secrete up to twice the amount of acid[4]. Beyond 5 mo of age however, there are progressive changes in gastric histology and physiology in these animals, with a reduction in acid secretion, such that at 12 mo they secrete less acid than wild-type controls, and by 20 mo they are essentially achlorhydric. This is associated with a progressive loss of gastric parietal cells and ECL cells over the same time period. Concomitant with these changes in the oxyntic mucosa, there is macroscopic evidence of hypertrophy in the gastric fundus and histological evidence of intestinal type metaplasia, a histological entity that is widely recognized as being premalignant. By 20 mo of age, there is evidence of gastric dysplasia in 100% and frank malignancy in 75% of mice. In comparison, wild-type FVB/N mice maintained under similar conditions did not develop metaplasia, dysplasia or gastric carcinoma[19].
Whilst INS-GAS mice developed gastric malignancies spontaneously over 2 years, it was also shown that this process was accelerated significantly by H felis infection. After 6 mo, there was significantly more gastric atrophy in all H felis-infected INS-GAS mice relative to both uninfected INS-GAS and H felis-infected FVB/N mice. In addition, there was also evidence of malignant progression, with 85% of infected INS-GAS mice being reported as showing at least intramucosal carcinoma after 6 mo of infection, in comparison to 12.5% of the uninfected INS-GAS group and none of the FVB/N groups[19]. Subsequent investigations have demonstrated that H pylori as well as H felis can induce gastric cancer in these mice, however there was a significant difference in susceptibility between male and female INS-GAS mice. After 7 mo of infection, four of 12 infected males were found to have gastric adenocarcinoma, whilst none of the other groups developed malignancies. In this study, progression to metaplasia and dysplasia was observed in all groups, but more severe changes were present in male than female animals[35].
The H felis-infected INS-GAS model has also been used to investigate the effects of administering the CCK-2 receptor inhibitor YF476. When this drug, in conjunction with the H2 receptor antagonist loxtidine, was given to INS-GAS mice infected with H felis, it significantly inhibited the development of gastric atrophy, dysplasia, and adenocarcinoma[36].
MTI/G-Gly and INS-GAS/MTI/G-gly: A third type of transgenic mouse that produces glycine extended gastrin has also been created by inserting two stop codons into the human gastrin gene after glycine-72. This transgene was spliced with the mouse metallothionein promoter to create transgenic animals that express the transgene in all tested tissue types and which constitutively overexpress glycine extended forms of gastrin[5]. This mouse model does not demonstrate a gastric phenotype histologically, and gastric tumors are not seen in the mice at 1 year of age[5]. In order to investigate whether glycine extended forms of gastrin modulated the effects of amidated gastrin upon the stomach, INS-GAS and MTI/G-Gly mice were crossed to generate doubly transgenic INS-GAS/MTI/G-Gly mice. These mice demonstrated less mucosal atrophy than INS-GAS mice and there was evidence of acid hypersecretion rather than the hypochlorhydria observed in INS-GAS mice. The altered phenotype of INS-GAS/MTI/G-Gly mice appeared to result from reduced gastric epithelial apoptosis rather than due to any changes in proliferation[37]. However, these changes in atrophy did not result in a reduction in malignant susceptibility, as at 18 mo all INS/GAS and all INS-GAS/MTI/G-Gly mice had developed gastric malignancies[37].
The consequences of gastrin deficiency in vivo have been investigated by a number of groups by generating gastrin knockout mice. Under normal animal house conditions, these animals develop gastric atrophy, with thinner gastric mucosae, fewer H+/K+ ATPase-positive parietal cells and impaired acid secretion[3839]. In addition, the oxyntic mucosa contains fewer chromogranin A immunopositive ECL cells and increased numbers of TFF-2-expressing cells, indicative of spasmolytic peptide expressing metaplasia (SPEM)[40]. Also, ECL cells appear to be clustered towards the bottom of the gastric gland of gastrin knockout mice and there is a reduced rate of parietal cell migration to the base of the gland in these animals[41].
The gastric phenotype of gastrin knockout[42] mice predisposes these animals to colonisation of the stomach with bacteria[43], resulting in inflammation and an initial increase in parietal and G-cell numbers[44]. The long term effect of this chronic inflammatory state may be to promote malignant transformation, and in some laboratories gastric tumors have been found in gastrin knockout mice by 1 year of age[4245]. When the specific effects of infection with H pylori strain 119/95 (a CagA positive, VacA positive strain previously shown to cause gastritis acutely[46], and gastric epithelial lymphomas with chronic infection in C57Bl/6 mice[47]) were investigated in these mice, there was an alteration in acid secretion, thought to be stimulated through a vagal response mechanism, but no increased risk of tumor development was observed at 6 mo[48].
CCK-2 receptor null mice have also been produced independently by two groups. These mice demonstrate marked gastric atrophy and reduced acid secretion as predicted[49–51]. There is also evidence of morphological changes in ECL cells, resulting in cells with loss of normal secretory vesicles and replacement with microvesicles and dense core granules[52]. As far as we are aware, there are no reports of increased susceptibility to gastric carcinogenesis in CCK-2 null animals.
Persistent hypergastrinemia can occur as a consequence of a number of different pathological states. These can broadly be divided into conditions which cause uncontrolled excess gastrin secretion such as gastrin-secreting tumors, and the normal physiological response to suppressed gastric acid secretion (Table 2). There is evidence that hypergastrinemia, particularly that which results from gastrinomas and chronic atrophic gastritis, may be associated with the development of gastric malignancies.
| Acidic gastric pH | Elevated gastric pH |
| Gastrinoma | Chronic atrophic gastritis |
| Antral predominant H pylori infection | Autoimmune |
| Pyloric obstruction | H pylori infection |
| Renal failure | Acid-suppressing medication |
| Retained gastric antrum following Billroth II gastrectomy | Vagotomy |
Neuroendocrine tumors of the pancreas and duodenum are rare, and are either functional, secreting one of a variety of neuropeptides, or non functioning, where elevated levels of neuropeptides are not detected. Of the functional tumors, the commonest hormone to be secreted is gastrin, accounting for up to 30% of such neoplasms. Gastrinomas have an incidence of 0.5-3 per million population per year[53] and were first described, along with a syndrome of gastric hypersecretion, in 1955 by Zollinger and Ellison[54]. The majority of gastrinomas are sporadic, however, approximately 12% are associated with the multiple endocrine neoplasia syndrome type 1 (MEN1)[55], in association with functional adenomas of the parathyroid (90%), pituitary [e.g. prolactinomas (17%)] and pancreas [e.g. insulinomas (10%)][56].
Unlike the first report by Zollinger and Ellison, in which one patient had radical surgery, but continued to secrete gastric acid and eventually died, and another required a total gastrectomy to control the adverse effects of gastric acid hypersecretion, today the prognosis for patients with gastrinoma is relatively good. The most important prognostic factor is the presence or absence of hepatic metastases. Patients without hepatic metastases at presentation (more than 75% of cases) have a 90%-100% 10-year survival, whilst those with metastatic disease have only a 10%-20% 10-year survival[53]. The advent of H2 receptor antagonists and subsequently PPIs has enabled control of gastric acid hypersecretion in the majority of patients, thereby reducing the risk of peptic ulceration. These therapies have made a significant impact upon the effects of ZES, however they target the consequences of hypergastrinemia rather than the underlying hormone production. Thus, surgery to remove the primary gastrinoma remains the only potentially curative option. This is feasible in at least 20%-45% of patients with sporadic ZES, but in far fewer patients with MEN1/ZES, as they are more likely to have multiple or diffuse tumors that are not amenable to surgery[53].
H pylori infection is an important independent risk factor for gastric carcinogenesis and gastric atrophy. Observational data suggest that H pylori infection directly causes mild degrees of hypergastrinemia. For example, asymptomatic patients with H pylori colonisation have been shown to have elevated serum gastrin concentrations relative to a control population, despite similar gastric acid output[57], while Levi et al[58] demonstrated that following H pylori eradication, there was a reduction in fasting serum gastrin concentration. It has also been demonstrated that following eradication of H pylori, there was an increase in somatostatin mRNA and a concomitant decrease in gastrin mRNA in patients with duodenal ulcers. This was associated with increased numbers of D-cells in the gastric corpus[59], suggesting that the hypergastrinemia caused by H pylori infection may result from a loss of somatostatin control over gastrin secretion.
Gastric atrophy is defined as the loss of parietal cell mass, leading to decreased acid secretion and consequent increased luminal pH. This interrupts the somatostatin negative feedback mechanism and results in hypergastrinemia. The most important causes of gastric atrophy are autoimmune (associated with pernicious anemia) and chronic H pylori infection. Both types of atrophic gastritis are associated with hypergastrinemia, although the fasting serum gastrin concentration is usually more markedly elevated in the autoimmune type, due to the more profound loss of parietal cells.
Autoimmune atrophic gastritis: The epidemiology of autoimmune atrophic gastritis is similar to that of other autoimmune diseases, with a female to male predominance approaching 2:1 and with individuals in their 7th decade or later being typically affected[60]. This condition is characterised by vitamin B12 deficiency as a result of loss of intrinsic factor and is associated with autoantibodies towards gastric parietal cells and/or intrinsic factor. These autoantibodies are found in the sera of 70% and 55% of patients with pernicious anemia respectively and at least one autoantibody is present in 85% of patients. Although it has been demonstrated that these antibodies can be cytotoxic in vitro[61], it is less clear whether they are the responsible for causing gastric atrophy in vivo.
H pylori-associated atrophic gastritis: The second important cause of gastric atrophy is chronic H pylori infection. Most commonly, primary infection occurs in childhood, hence many patients have long-term colonization of the stomach. This can have a number of consequences, ranging from increased gastric acid secretion and associated peptic ulcer disease to gastric atrophy with resultant increased luminal pH. The latter is associated with an increased risk of gastric cancer. The factors that influence the clinical outcomes of H pylori infection in individual patients remain poorly understood. The site of colonization within the stomach appears to be important however, with antral infections being particularly associated with peptic ulcer disease, whereas gastric corpus colonization is more likely to lead to gastric atrophy.
H pylori occupies a niche in the mucus layer of the gastric mucosa and produces urease enzymes which allow the pH of the immediate environment to be raised to physiological levels, thus facilitating prolonged colonization. Various bacterial, host and environmental factors have been suggested to influence the response to H pylori infection. For example, mouse models have demonstrated that polarization of the immunological response towards a Th1 type increases the risk of developing gastric atrophy and subsequent gastric cancer[62], while genetic studies have suggested that polymorphisms in immune-response genes may also influence the consequences of infection in human subjects[63].
H pylori is associated with gastric autoimmunity, although the specific mechanisms involved are not yet fully understood. Presotto et al[64] demonstrated that 58% of 79 asymptomatic patients with detectable anti-parietal cell antibodies had serological or histological evidence of H pylori infection compared to 39% of a control population (P = 0.03). It has also been proposed that early gastric autoimmunity may be reversible when concomitant H pylori infection is treated[65]. The precise interactions between H pylori infection and the development of autoimmune gastritis therefore warrant further investigation.
The hypergastrinemia which results from the causes described above is associated with increased risks of developing various different gastric tumors.
Hypergastrinemia in the absence of H pylori infection is most strongly associated with the development of gastric neuroendocrine tumors. In contrast, the hypergastrinemia associated with chronic H pylori infection may act as a co-factor during the development of gastric adenocarcinoma. In the following section, we will discuss the role of gastrin in the pathogenesis, diagnosis, and treatment of these specific gastric tumor types.
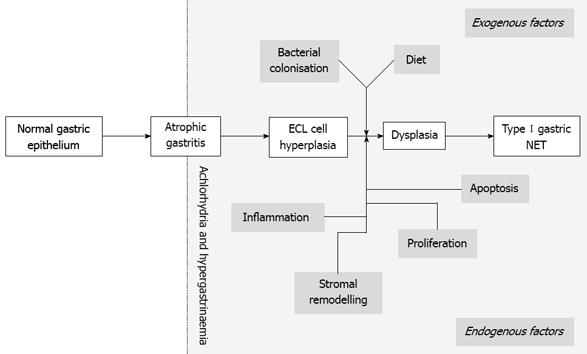
Pathogenesis: Gastric neuroendocrine (carcinoid) tumors are the classical example of gastrin-induced malignancies. These neoplasms are derived from ECL cells, which are the most abundant neuroendocrine cell type in the oxyntic mucosa. Hypergastrinemia alone appears to be sufficient to induce ECL cell hyperplasia, however, for macroscopic neuroendocrine tumor formation, additional triggers are required. For example, lifelong therapy of rats with PPIs resulted in the development of ECL cell tumors[66], whereas the same has not been observed in humans despite induction of hypergastrinemia[1314]. This suggests that additional host or environmental factors are required for tumor development.
The typical conditions in which ECL tumors develop are either gastric atrophy associated with pernicious anemia (type I gastric neuroendocrine tumors), or the presence of prolonged hypergastrinemia and mutation of the MEN1 gene in ZES associated with MEN type I (type II gastric neuroendocrine tumors)[67] (Table 3). The latter condition provides further evidence that hypergastrinemia alone may be insufficient to cause gastric neuroendocrine tumors, as the relative risk for developing such neoplasms is at least 70 fold lower in patients with sporadic ZES compared with those who have ZES associated with MEN1[68].
| Type | Associated diseases | Proportion of gastric NETs | Typical endoscopic findings | Plasma gastrin | Gastric juice pH | Prognosis |
| I | Chronic autoimmune atrophic gastritis | 80% | Multiple < 1 cm polyps | High | ~7 | Good |
| II | ZES and MEN1 | 5% | Multiple < 1 cm polyps | High | < 2 | Variable |
| III | None | 15% | Single 2-5 cm polyp | Unchanged | 1-2 | Poor |
In pernicious anemia, there is a reduction in the number of gastric parietal cells and subsequent achlorhydria. This affects the somatostatin feedback loop that controls gastrin secretion, thereby rendering the patient hypergastrinemic. Hypergastrinemia then provides a proliferative drive to ECL cells (Figure 3). The achlorhydric environment also provides opportunities for further microenvironmental changes, including the provision of a niche for bacterial colonization. Interest in this aspect of gastric carcinogenensis has been present since the 1980s, when numerous studies demonstrated increased levels of N-nitroso compounds (potential carcinogens that are metabolised by intra gastric bacteria from nitrosamines) in the gastric lumens of patients with both atrophic gastritis and gastric malignancy[69].
The major risk factor in addition to hypergastrinemia that promotes the development of type II gastric neuroendocrine tumors is mutation of the MEN1 gene. Gastric neuroendocrine tumors are seen in less than 1% of patients with sporadic ZES, whilst in those with ZES associated with MEN type I, the prevalence is 13%-43%[70]. A recent prospective study of 57 consecutive hypergastrinemic MEN1 patients reported that 100% had abnormal ECL cell distribution and 23% had gastric neuroendocrine tumors.
The MEN1 gene encodes a 610-amino-acid protein, menin. Menin is expressed in many diverse tissue types and is localized in the nucleus. It binds directly to DNA in a sequence-independent manner and is also capable of binding several other nuclear factors including transcription factors and DNA repair proteins. The physiological function of menin is as a tumor suppressor, although the specific mechanism of action is less clear. The mutations seen in the MEN1 gene result in either reduced expression of menin or in some cases complete absence of menin[56].
Interestingly, local rather than somatic mutations of menin may also be of significance in the pathogenesis of type I gastric carcinoids and two studies have assessed loss of heterozygosity (LOH) of 11q13, the locus for the MEN1 gene, in this tumor type. The smaller study assessed three gastric neuroendocrine cell tumors and demonstrated LOH at this locus in two patients and a localized mutation of MEN1 in one[71]. The larger study investigated 17 type I gastric neuroendocrine tumors, four type III gastric neuroendocrine tumors and two histologically defined neuroendocrine carcinomas. 47.1% of type I neuroendocrine tumors had LOH at 11q13 compared to 25% of the type III neuroendocrine tumors, while both neuroendocrine carcinomas showed substantial deletions at this locus[72].
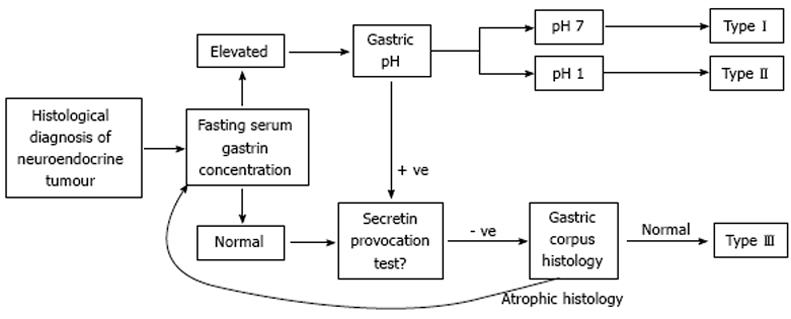
Diagnosis: Clearly, measurement of fasting serum gastrin concentration is an important component in the diagnostic pathway for patients with gastric neuroendocrine tumors. Once a histological diagnosis of gastric neuroendocrine tumor has been made, it is imperative to ascertain the type of tumor, as well as its stage, as this will influence treatment. Defining the type of tumor can be achieved in most cases by measuring the fasting serum gastrin concentration along with the pH of gastric juice (Figure 4). In the presence of a normal or low fasting serum gastrin concentration, a diagnosis of sporadic or type III gastric neuroendocrine tumor is most likely. In the context of an elevated serum gastrin concentration, the gastric juice pH determines whether a type I lesion (neutral pH) or type II lesion (acidic pH) is present. This simple algorithm provides the initial data that inform future investigations. Many of these lesions are still gastrin sensitive at the time of diagnosis, and in such cases, removal of the source of hypergastrinemia by antrectomy (type I) or gastrinoma resection (type II) should result in tumor regression. To investigate whether a type I gastric neuroendocrine tumor is gastrin sensitive, it may be useful to perform an octreotide suppression test. This involves biopsying the gastric corpus mucosa and neuroendocrine tumors pre and post octreotide infusion and assessing whether there is a reduction in mRNA abundance for the secretory components of ECL cells, such as histidine decarboxylase, following octreotide administration. This surrogate is then used as a marker for gastrin sensitivity[73].
Treatment: Those type I and II gastric neuroendocrine tumors that retain gastrin sensitivity may be amenable to treatment by methods which reduce elevated serum gastrin concentrations. This may involve locating and excising a primary gastrinoma in the case of a type II gastric neuroendocrine tumor, or surgical antrectomy in a patient with pernicious anemia and autoimmune chronic atrophic gastritis. Very occasionally, large type I gastric carcinoids grow autonomously and are no longer gastrin-sensitive, and such tumors may require gastrectomy. Future treatments for types 1 and 2 neuroendocrine tumors may include the use of CCK-2 receptor antagonists to inhibit the effects of elevated serum gastrin concentrations.
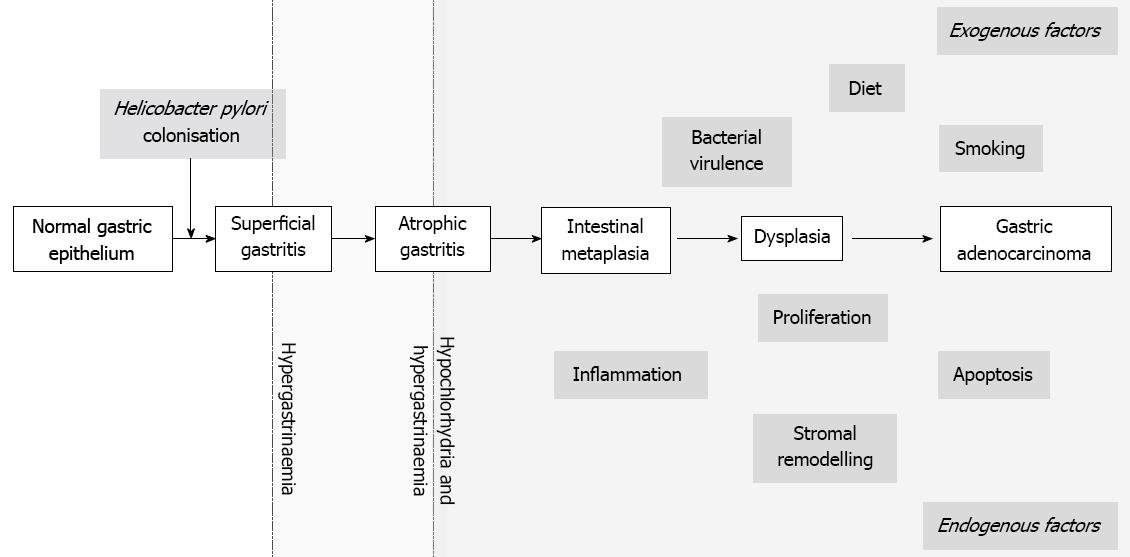
Pathogenesis: Gastric adenocarcinoma accounts for the greatest mortality and morbidity associated with primary malignancies of the gastric mucosa. It develops through a stereotypical pathological sequence[74] characterized by progression from chronic active gastritis to atrophic gastritis, and via metaplastic lesions to dysplasia and malignancy (Figure 5). As described above, gastrin secretion is altered following Helicobacter infection. There is accumulating evidence, particularly from the INS-GAS animal model described above, that hypergastrinemia may contribute towards the development of gastric atrophy and remodelling of the gastric mucosa. However, it is currently not clear to what extent inferences about human gastric carcinogenesis can be made from the observations in these transgenic mice.
Diagnosis: Measurement of fasting serum gastrin concentration is reasonably simple and therefore several groups have investigated whether such assessment assists in the diagnosis or helps to determine the management of gastric cancer. Although a statistically significant elevation in serum gastrin concentration has been demonstrated in patients with gastric cancer compared to controls[7576], the clinical usefulness of such assessment is currently limited. Attempts to use fasting serum gastrin concentration either as a marker of prognosis and resectability[77] or as a part of a panel of surrogate markers for initial diagnosis[78] have also been unsuccessful, and such approaches have largely been superceded by advancements in endoscopy and imaging techniques.
More recently, assessment of serum gastrin concentration has been evaluated as part of a panel of potential biomarkers for determining the presence and location of gastric atrophy. A Swedish population of 1000 individuals between the ages of 20-80 years underwent gastroscopy with biopsies taken from the antrum, corpus and fundus to assess for the presence of atrophy and at the same time had blood taken for analysis of gastrin-17, H pylori IgG antibody, pepsinogen I and II. This panel had a relatively high false positive result of 31%, although the authors defended this finding by emphasizing the potential pitfalls of sampling error when relying on histological assessment of small mucosal biopsies. Indeed, they asserted that the finding of serological markers in keeping with atrophy in 4.9% of patients with histological evidence of H pylori-associated non-atrophic gastritis, compared to just 0.8% of H pylori-negative patients who had no histological evidence of atrophy, potentially demonstrates the strength of serology as a global marker of atrophy rather than being limited to samples obtained from a small geographic area. Taking histology as the gold standard, these biomarkers diagnosed corpus atrophy with a positive predictive value of 69% (CI 95%: 66-72%) and a negative predictive value of 98% (95% CI: 97-99%) in this population[79].
Hansen et al[80] recently investigated a cohort of 101 601 patients from whom serum samples were collected in Sweden in the 1970s. They compared 230 patients who developed gastric cancer by 1992 with controls from the same cohort, and demonstrated a significant correlation between elevated serum gastrin concentration and low serum pepsinogen I/II ratios, and increased risk of developing non-cardia gastric cancer. They also demonstrated that most cases of gastric cardia cancer were not associated with Helicobacter infection, and did not show an association with markers of gastric atrophy; however, a minority of cases had serological evidence of past or present Helicobacter infection and an association with markers of gastric atrophy. This suggests that gastric cardia cancers develop most commonly through a Helicobacter/gastrin-independent mechanism, with a small subset having a similar etiology to non-cardia cancers.
The same panel of biomarkers have also been assessed in other cohorts, including a pediatric population, but in this case, they were found to be insufficiently sensitive to diagnose Helicobacter infection or the low incidence of atrophy that is present in this population[81]. Endoscopic evaluation of the upper GI tract therefore remains the accepted gold standard for the assessment of mucosal lesions of the GI tract; however, there may be a role, which needs further investigation, for a panel of biomarkers such as those described above in identifying adults at particularly high risk of gastric atrophy.
Treatment: Various groups have assessed whether immunohistochemical analysis of gastric carcinoma tissue for the presence of gastrin and/or the CCK-2 receptor is useful for predicting prognosis. Normal gastric mucosa expresses the CCK-2 receptor on ECL cells and parietal cells. Immunohistochemical studies using archival samples have shown that as the Correa sequence progresses, with development of gastric atrophy and parietal cell loss, an increased percentage of cells in the gastric corpus express the CCK-2 receptor[82]. In normal gastric corpus mucosa, gastrin immunopositive cells are not detectable; however, with progression down the Correa sequence, increased expression of gastrin and its precursors have been observed[82]. An immunohistochemical study based on a tissue array of 304 gastric cancer resection specimens from Korea demonstrated that 56.5% expressed CCK-2 receptors within the malignant tissue and that gastrin was detectable within the tumor mass in 47.7%[83]. A Welsh study has also demonstrated adverse survival in patients whose gastric tumors stained positively for gastrin[84]. These observations suggest that gastrin may represent a potential therapeutic target for the prevention or treatment of gastric carcinoma. Initial attempts at targeting gastrin to improve survival in gastric cancer used proglumide, a weak CCK-2 receptor inhibitor, and a randomized controlled trial demonstrated no survival benefit following treatment with this drug[85]. Subsequent developments have included the development of G17DT, an immunogenic mimic of gastrin 17 that causes the production of anti-gastrin antibodies[86]. Immunization with this agent improved the survival of severe combined immune deficient (SCID) mice xenografted with the human gastric cancer cell line, MGLVA1asc, and this effect was equivalent to combination chemotherapy with 5-FU and leucovorin. Moreover, the use of 5-FU in conjunction with G17DT appeared to have an additive effect[87]. G17DT was well tolerated in phase II clinical trials[88], hence a multicenter phase II trial of G17DT in conjunction with 5-FU and cisplatin in advanced gastric cancer has recently been performed. 60% of G17DT treated patients successfully developed anti-gastrin-17 antibodies and this subgroup showed significantly improved survival[89].
MALT lymphomas are marginal zone lymphomas derived from the mucosa-associated lymphoid tissue of the stomach. They occur in patients with gastric atrophy and are strongly associated with H pylori infection. MALT lymphomas are associated with both hypergastrinemia and overexpression of the CCK-2 receptor in the gastric mucosa. The presence of hypergastrinemia is not surprising in view of the association with gastric atrophy, but the overexpression of CCK-2 receptor suggests a potential mechanism through which gastrin may exert a trophic effect in this tumor type[9091].
These lesions are found in the oxyntic mucosa and are described by the World Health Organization as a proliferation of surface foveolar cells lining elongated, distorted pits that extend deep into the stroma. They show hyperplasia of mucous neck cells and variable amounts of cystic dilatation[92]. Although they are not intrinsically dysplastic, progression to gastric malignancy has been reported, particularly when there is underlying familial adenomatous polyposis or juvenile polyposis. Patients with these conditions have fundic cystic gland polyps on endoscopy in up to 90%[93] of cases and of these polyps, up to 40%-50%[9394] have associated dysplasia.
Patients without inherited polyposis syndromes, however, account for the vast majority of those with fundic cystic gland polyps. In this group, the association between polyps and dysplasia is far less clear cut. Although dysplasia and cancers have been reported in patients who have these lesions[95–97], it is not clear whether the incidence of malignancy is significantly higher than that of the normal population.
The association between fundic gland polyps and gastrin is derived from the recognition that these lesions occur more commonly in patients who are taking long-term PPIs. However, PPI-induced fundic cystic gland polyps probably have a different etiology compared to the sporadic polyps that occur in patients who are not taking PPIs (which are associated with somatic mutations in β-catenin[929697]) and the polyps associated with FAP or juvenile polyposis, where there are known molecular aberrations. It has been suggested that PPI-induced fundic cystic gland polyps arise as a result of impaired glandular flow after hypergastrinemia-induced parietal cell hyperplasia has caused a mechanical obstruction to the gland[98]. However, this does not appear to be related to the severity of hypergastrinemia, as a small Norwegian study has shown equivalent degrees of hypergastrinemia in patients taking PPIs with and without fundic gland polyps[99].
In the context of PPI usage, the risk of malignant transformation is extremely low and there is at present no recommendation either for endoscopic removal of lesions or for any form of endoscopic surveillance in patients with fundic cystic gland polyps who are taking PPIs, unless they also have a familial polyposis syndrome[98].
Evidence therefore suggests that gastrin may affect the risk of developing various epithelial and possibly lymphoid gastric malignancies by altering key cellular pathways including proliferation, apoptosis, migration, tissue remodelling and possibly angiogenesis. Gastrin is also a potential therapeutic target for the treatment of various gastric tumors. For example, surgical approaches to correct hypergastrinemia may be employed for some gastric neuroendocrine tumors, while agents such as G17DT have shown some promise in phase II clinical trials in advanced gastric adenocarcinoma[89]. Such approaches may also have future uses in the prevention of malignancy, for example in patients who have precursor lesions such as ECL cell hyperplasia or gastric atrophy. If such therapies prove effective, there may additionally be a need to reconsider the role of endoscopic surveillance for gastric atrophy, an approach that has lost favor recently.
In population terms, more people are hypergastrinemic than ever before as a result of continued increases in the prescription rates of PPI drugs. In comparison to the numbers of individuals prescribed these drugs, gastrin-associated malignancies are undoubtedly rare, however, there is an ongoing debate about the safety profile of these agents[98100–102].
Animal studies have shown that ECL cell hyperplasia can occur in response to hypergastrinemia induced by chronic proton pump inhibition[12]. In rats that were rendered achlorhydric for their entire lifespan, ECL-cell-derived neuroendocrine tumors also developed[66]. However, there is no convincing evidence that PPIs cause ECL cell malignancies in humans, possibly because PPIs do not usually induce complete achlorhydria[103]. Although no tumors have been found, there is evidence of diffuse and linear patterns of ECL cell hyperplasia in patients treated for a decade with PPIs[13–14, 104] .
There has also been concern about whether PPI treatment modulates the consequences of chronic H pylori infection. Recent studies have compared patients treated with anti-reflux surgery and those treated with PPIs. In patients who were H pylori-negative, treatment for 7 years with a PPI made no difference to mucosal inflammation or atrophy. However, patients who were H pylori-positive over the same 7-year period showed increased progression towards mucosal atrophy and increased inflammation if treated with a PPI, in comparison to those treated with surgery[104]. Although this suggests that H pylori infection should be eradicated before initiating chronic acid suppression therapy, the observed changes were modest and to date there has been no evidence of progression beyond mucosal atrophy. The studies were not designed to assess whether there was any associated increase in the incidence of gastric cancer, and much larger cohorts would be required to investigate this. Epidemiological database studies have been cited as demonstrating that PPI prescription is associated with an increased risk of gastric cancer[98]. However these data remain unpublished and this type of retrospective analysis cannot reliably distinguish patients who have been prescribed PPIs for the presenting symptoms of gastric cancer from any increase in the incidence of gastric carcinoma as a result of PPI use.
Current evidence therefore suggests that the relatively modest hypergastrinemia induced by PPI drugs is not associated with malignant transformation in the human stomach. When considering the overall safety profile of this class of drugs, gastrin-independent adverse effects such as malabsorption of vitamin B12[105–110] should also be considered. Although CCK-2 receptor inhibition or combined PPI and CCK-2 receptor inhibition have been suggested as potential ways of reducing the gastrin-mediated side effects of PPIs, it seems unlikely that this approach will be clinically useful whilst PPIs have such a good safety profile, and especially as some of the adverse effects are probably related to hypochlorhydria rather than hypergastrinemia.
Our understanding of the importance of gastrin in gastric tumorigenesis has therefore increased significantly over recent years and the generation of transgenic animal models has greatly facilitated our understanding of the mechanisms involved. Issues that still need clarification include the precise role of gastrin in the pathogenesis of human gastric adenocarcinoma, whether pharmacological targeting of gastrin or its receptor is beneficial for the treatment and/or prevention of various gastric tumors and whether PPI-induced hypergastrinemia has any long term clinically important consequences, particularly in the context of chronic H pylori infection.
| 1. | Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74-108. [Cited in This Article: ] |
| 2. | Edkins JS. The chemical mechanism of gastric secretion. J Physiol. 1906;34:133-144. [Cited in This Article: ] |
| 3. | Dockray GJ, Varro A, Dimaline R, Wang T. The gastrins: their production and biological activities. Annu Rev Physiol. 2001;63:119-139. [Cited in This Article: ] |
| 4. | Wang TC, Koh TJ, Varro A, Cahill RJ, Dangler CA, Fox JG, Dockray GJ. Processing and proliferative effects of human progastrin in transgenic mice. J Clin Invest. 1996;98:1918-1929. [Cited in This Article: ] |
| 5. | Koh TJ, Dockray GJ, Varro A, Cahill RJ, Dangler CA, Fox JG, Wang TC. Overexpression of glycine-extended gastrin in transgenic mice results in increased colonic proliferation. J Clin Invest. 1999;103:1119-1126. [Cited in This Article: ] |
| 6. | Buchan AM, Squires PE, Ring M, Meloche RM. Mechanism of action of the calcium-sensing receptor in human antral gastrin cells. Gastroenterology. 2001;120:1128-1139. [Cited in This Article: ] |
| 7. | Schmitz F, Göke MN, Otte JM, Schrader H, Reimann B, Kruse ML, Siegel EG, Peters J, Herzig KH, Fölsch UR. Cellular expression of CCK-A and CCK-B/gastrin receptors in human gastric mucosa. Regul Pept. 2001;102:101-110. [Cited in This Article: ] |
| 8. | Willems G, Vansteenkiste Y, Limbosch JM. Stimulating effect of gastrin on cell proliferation kinetics in canine fundic mucosa. Gastroenterology. 1972;62:583-589. [Cited in This Article: ] |
| 9. | Kidd M, Tang LH, Modlin IM, Zhang T, Chin K, Holt PR, Moss SF. Gastrin-mediated alterations in gastric epithelial apoptosis and proliferation in a mastomys rodent model of gastric neoplasia. Digestion. 2000;62:143-151. [Cited in This Article: ] |
| 10. | Hansen OH, Pedersen T, Larsen JK, Rehfeld JF. Effect of gastrin on gastric mucosal cell proliferation in man. Gut. 1976;17:536-541. [Cited in This Article: ] |
| 11. | Bordi C, Cocconi G, Togni R, Vezzadini P, Missale G. Gastric endocrine cell proliferation. Association with Zollinger-Ellison syndrome. Arch Pathol. 1974;98:274-278. [Cited in This Article: ] |
| 12. | Larsson H, Carlsson E, Mattsson H, Lundell L, Sundler F, Sundell G, Wallmark B, Watanabe T, Håkanson R. Plasma gastrin and gastric enterochromaffinlike cell activation and proliferation. Studies with omeprazole and ranitidine in intact and antrectomized rats. Gastroenterology. 1986;90:391-399. [Cited in This Article: ] |
| 13. | Lamberts R, Brunner G, Solcia E. Effects of very long (up to 10 years) proton pump blockade on human gastric mucosa. Digestion. 2001;64:205-213. [Cited in This Article: ] |
| 14. | Singh P, Indaram A, Greenberg R, Visvalingam V, Bank S. Long term omeprazole therapy for reflux esophagitis:follow-up in serum gastrin levels,EC cell hyperplasia and neoplasia. World J Gastroenterol. 2000;6:789-792. [Cited in This Article: ] |
| 15. | Sun WH, Zhu F, Chen GS, Su H, Luo C, Zhao QS, Zhang Y, Shao Y, Sun J, Zhou SM. Blockade of cholecystokinin-2 receptor and cyclooxygenase-2 synergistically induces cell apoptosis, and inhibits the proliferation of human gastric cancer cells in vitro. Cancer Lett. 2008;263:302-311. [Cited in This Article: ] |
| 16. | Song DH, Rana B, Wolfe JR, Crimmins G, Choi C, Albanese C, Wang TC, Pestell RG, Wolfe MM. Gastrin-induced gastric adenocarcinoma growth is mediated through cyclin D1. Am J Physiol Gastrointest Liver Physiol. 2003;285:G217-G222. [Cited in This Article: ] |
| 17. | Varro A, Noble PJ, Wroblewski LE, Bishop L, Dockray GJ. Gastrin-cholecystokinin(B) receptor expression in AGS cells is associated with direct inhibition and indirect stimulation of cell proliferation via paracrine activation of the epidermal growth factor receptor. Gut. 2002;50:827-833. [Cited in This Article: ] |
| 18. | Dickson JH, Grabowska A, El-Zaatari M, Atherton J, Watson SA. Helicobacter pylori can induce heparin-binding epidermal growth factor expression via gastrin and its receptor. Cancer Res. 2006;66:7524-7531. [Cited in This Article: ] |
| 19. | Wang TC, Dangler CA, Chen D, Goldenring JR, Koh T, Raychowdhury R, Coffey RJ, Ito S, Varro A, Dockray GJ. Synergistic interaction between hypergastrinemia and Helicobacter infection in a mouse model of gastric cancer. Gastroenterology. 2000;118:36-47. [Cited in This Article: ] |
| 20. | Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759-767. [Cited in This Article: ] |
| 21. | Houghton J, Stoicov C, Nomura S, Rogers AB, Carlson J, Li H, Cai X, Fox JG, Goldenring JR, Wang TC. Gastric cancer originating from bone marrow-derived cells. Science. 2004;306:1568-1571. [Cited in This Article: ] |
| 22. | Cui G, Takaishi S, Ai W, Betz KS, Florholmen J, Koh TJ, Houghton J, Pritchard DM, Wang TC. Gastrin-induced apoptosis contributes to carcinogenesis in the stomach. Lab Invest. 2006;86:1037-1051. [Cited in This Article: ] |
| 23. | Przemeck SM, Varro A, Berry D, Steele I, Wang TC, Dockray GJ, Pritchard DM. Hypergastrinemia increases gastric epithelial susceptibility to apoptosis. Regul Pept. 2008;146:147-156. [Cited in This Article: ] |
| 24. | Ramamoorthy S, Stepan V, Todisco A. Intracellular mechanisms mediating the anti-apoptotic action of gastrin. Biochem Biophys Res Commun. 2004;323:44-48. [Cited in This Article: ] |
| 25. | Todisco A, Ramamoorthy S, Witham T, Pausawasdi N, Srinivasan S, Dickinson CJ, Askari FK, Krametter D. Molecular mechanisms for the antiapoptotic action of gastrin. Am J Physiol Gastrointest Liver Physiol. 2001;280:G298-G307. [Cited in This Article: ] |
| 26. | Pritchard DM, Berry D, Przemeck SM, Campbell F, Edwards SW, Varro A. Gastrin increases mcl-1 expression in type I gastric carcinoid tumors and a gastric epithelial cell line that expresses the CCK-2 receptor. Am J Physiol Gastrointest Liver Physiol. 2008;295:G798-G805. [Cited in This Article: ] |
| 27. | Chen CN, Hsieh FJ, Cheng YM, Chang KJ, Lee PH. Expression of inducible nitric oxide synthase and cyclooxygenase-2 in angiogenesis and clinical outcome of human gastric cancer. J Surg Oncol. 2006;94:226-233. [Cited in This Article: ] |
| 28. | Subramaniam D, Ramalingam S, May R, Dieckgraefe BK, Berg DE, Pothoulakis C, Houchen CW, Wang TC, Anant S. Gastrin-mediated interleukin-8 and cyclooxygenase-2 gene expression: differential transcriptional and posttranscriptional mechanisms. Gastroenterology. 2008;134:1070-1082. [Cited in This Article: ] |
| 29. | Konturek PC, Rembiasz K, Konturek SJ, Stachura J, Bielanski W, Galuschka K, Karcz D, Hahn EG. Gene expression of ornithine decarboxylase, cyclooxygenase-2, and gastrin in atrophic gastric mucosa infected with Helicobacter pylori before and after eradication therapy. Dig Dis Sci. 2003;48:36-46. [Cited in This Article: ] |
| 30. | Clarke PA, Dickson JH, Harris JC, Grabowska A, Watson SA. Gastrin enhances the angiogenic potential of endothelial cells via modulation of heparin-binding epidermal-like growth factor. Cancer Res. 2006;66:3504-3512. [Cited in This Article: ] |
| 31. | Wroblewski LE, Pritchard DM, Carter S, Varro A. Gastrin-stimulated gastric epithelial cell invasion: the role and mechanism of increased matrix metalloproteinase 9 expression. Biochem J. 2002;365:873-879. [Cited in This Article: ] |
| 32. | Varro A, Kenny S, Hemers E, McCaig C, Przemeck S, Wang TC, Bodger K, Pritchard DM. Increased gastric expression of MMP-7 in hypergastrinemia and significance for epithelial-mesenchymal signaling. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1133-G1140. [Cited in This Article: ] |
| 33. | Noble PJ, Wilde G, White MR, Pennington SR, Dockray GJ, Varro A. Stimulation of gastrin-CCKB receptor promotes migration of gastric AGS cells via multiple paracrine pathways. Am J Physiol Gastrointest Liver Physiol. 2003;284:G75-G84. [Cited in This Article: ] |
| 34. | Wang TC, Bonner-Weir S, Oates PS, Chulak M, Simon B, Merlino GT, Schmidt EV, Brand SJ. Pancreatic gastrin stimulates islet differentiation of transforming growth factor alpha-induced ductular precursor cells. J Clin Invest. 1993;92:1349-1356. [Cited in This Article: ] |
| 35. | Fox JG, Rogers AB, Ihrig M, Taylor NS, Whary MT, Dockray G, Varro A, Wang TC. Helicobacter pylori-associated gastric cancer in INS-GAS mice is gender specific. Cancer Res. 2003;63:942-950. [Cited in This Article: ] |
| 36. | Takaishi S, Cui G, Frederick DM, Carlson JE, Houghton J, Varro A, Dockray GJ, Ge Z, Whary MT, Rogers AB. Synergistic inhibitory effects of gastrin and histamine receptor antagonists on Helicobacter-induced gastric cancer. Gastroenterology. 2005;128:1965-1983. [Cited in This Article: ] |
| 37. | Cui G, Koh TJ, Chen D, Zhao CM, Takaishi S, Dockray GJ, Varro A, Rogers AB, Fox JG, Wang TC. Overexpression of glycine-extended gastrin inhibits parietal cell loss and atrophy in the mouse stomach. Cancer Res. 2004;64:8160-8166. [Cited in This Article: ] |
| 38. | Koh TJ, Goldenring JR, Ito S, Mashimo H, Kopin AS, Varro A, Dockray GJ, Wang TC. Gastrin deficiency results in altered gastric differentiation and decreased colonic proliferation in mice. Gastroenterology. 1997;113:1015-1025. [Cited in This Article: ] |
| 39. | Friis-Hansen L, Sundler F, Li Y, Gillespie PJ, Saunders TL, Greenson JK, Owyang C, Rehfeld JF, Samuelson LC. Impaired gastric acid secretion in gastrin-deficient mice. Am J Physiol. 1998;274:G561-G568. [Cited in This Article: ] |
| 40. | Nomura S, Yamaguchi H, Ogawa M, Wang TC, Lee JR, Goldenring JR. Alterations in gastric mucosal lineages induced by acute oxyntic atrophy in wild-type and gastrin-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2005;288:G362-G375. [Cited in This Article: ] |
| 41. | Kirton CM, Wang T, Dockray GJ. Regulation of parietal cell migration by gastrin in the mouse. Am J Physiol Gastrointest Liver Physiol. 2002;283:G787-G793. [Cited in This Article: ] |
| 42. | Friis-Hansen L, Rieneck K, Nilsson HO, Wadström T, Rehfeld JF. Gastric inflammation, metaplasia, and tumor development in gastrin-deficient mice. Gastroenterology. 2006;131:246-258. [Cited in This Article: ] |
| 43. | Sun FJ, Kaur S, Ziemer D, Banerjee S, Samuelson LC, De Lisle RC. Decreased gastric bacterial killing and up-regulation of protective genes in small intestine in gastrin-deficient mouse. Dig Dis Sci. 2003;48:976-985. [Cited in This Article: ] |
| 44. | Zavros Y, Rieder G, Ferguson A, Samuelson LC, Merchant JL. Genetic or chemical hypochlorhydria is associated with inflammation that modulates parietal and G-cell populations in mice. Gastroenterology. 2002;122:119-133. [Cited in This Article: ] |
| 45. | Zavros Y, Eaton KA, Kang W, Rathinavelu S, Katukuri V, Kao JY, Samuelson LC, Merchant JL. Chronic gastritis in the hypochlorhydric gastrin-deficient mouse progresses to adenocarcinoma. Oncogene. 2005;24:2354-2366. [Cited in This Article: ] |
| 46. | Wang X, Willén R, Wadström T, Aleljung P. RAPD-PCR, Histopathological and Serological Analysis of Four Mouse Strains Infected with Multiple Strains of Helicobacter pylori. Microb Ecol Health Dis. 1999;10:148-154. [Cited in This Article: ] |
| 47. | Wang X, Willén R, Andersson C, Wadström T. Development of high-grade lymphoma in Helicobacter pylori-infected C57BL/6 mice. APMIS. 2000;108:503-508. [Cited in This Article: ] |
| 48. | Zhao CM, Wang X, Friis-Hansen L, Waldum HL, Halgunset J, Wadström T, Chen D. Chronic Helicobacter pylori infection results in gastric hypoacidity and hypergastrinemia in wild-type mice but vagally induced hypersecretion in gastrin-deficient mice. Regul Pept. 2003;115:161-170. [Cited in This Article: ] |
| 49. | Nagata A, Ito M, Iwata N, Kuno J, Takano H, Minowa O, Chihara K, Matsui T, Noda T. G protein-coupled cholecystokinin-B/gastrin receptors are responsible for physiological cell growth of the stomach mucosa in vivo. Proc Natl Acad Sci USA. 1996;93:11825-11830. [Cited in This Article: ] |
| 50. | Langhans N, Rindi G, Chiu M, Rehfeld JF, Ardman B, Beinborn M, Kopin AS. Abnormal gastric histology and decreased acid production in cholecystokinin-B/gastrin receptor-deficient mice. Gastroenterology. 1997;112:280-286. [Cited in This Article: ] |
| 51. | Rindi G, Langhans N, Rehfeld JF, Beinborn M, Kopin AS. Abnormal gastric morphology and function in CCK-B/gastrin receptor-deficient mice. Yale J Biol Med. 1998;71:347-354. [Cited in This Article: ] |
| 52. | Chen D, Zhao CM, Al-Haider W, Håkanson R, Rehfeld JF, Kopin AS. Differentiation of gastric ECL cells is altered in CCK(2) receptor-deficient mice. Gastroenterology. 2002;123:577-585. [Cited in This Article: ] |
| 53. | Jensen RT, Niederle B, Mitry E, Ramage JK, Steinmuller T, Lewington V, Scarpa A, Sundin A, Perren A, Gross D. Gastrinoma (duodenal and pancreatic). Neuroendocrinology. 2006;84:173-182. [Cited in This Article: ] |
| 54. | Zollinger RM, Ellison EH. Primary peptic ulcerations of the jejunum associated with islet cell tumors of the pancreas. Ann Surg. 1955;142:709-723; discussion, 724-728. [Cited in This Article: ] |
| 55. | Ito T, Tanaka M, Sasano H, Osamura YR, Sasaki I, Kimura W, Takano K, Obara T, Ishibashi M, Nakao K. Preliminary results of a Japanese nationwide survey of neuroendocrine gastrointestinal tumors. J Gastroenterol. 2007;42:497-500. [Cited in This Article: ] |
| 56. | Piecha G, Chudek J, Wiecek A. Multiple Endocrine Neoplasia type 1. Eur J Intern Med. 2008;19:99-103. [Cited in This Article: ] |
| 57. | Smith JT, Pounder RE, Nwokolo CU, Lanzon-Miller S, Evans DG, Graham DY, Evans DJ Jr. Inappropriate hypergastrinaemia in asymptomatic healthy subjects infected with Helicobacter pylori. Gut. 1990;31:522-525. [Cited in This Article: ] |
| 58. | Levi S, Beardshall K, Swift I, Foulkes W, Playford R, Ghosh P, Calam J. Antral Helicobacter pylori, hypergastrinaemia, and duodenal ulcers: effect of eradicating the organism. BMJ. 1989;299:1504-1505. [Cited in This Article: ] |
| 59. | Moss SF, Legon S, Bishop AE, Polak JM, Calam J. Effect of Helicobacter pylori on gastric somatostatin in duodenal ulcer disease. Lancet. 1992;340:930-932. [Cited in This Article: ] |
| 60. | Carmel R. Prevalence of undiagnosed pernicious anemia in the elderly. Arch Intern Med. 1996;156:1097-1100. [Cited in This Article: ] |
| 61. | Kogawa K. Parietal cell antibodies. Part II. Cytotoxic activities of parietal cell antibodies. Experiment 1. The observations on cytotoxic activities of parietal cell antibodies to normal human parietal cells in vitro. Experiment 2. The histochemical changes of rat stomach after administrations of rabbit anti-rat gastric mucosa sera. Gastroenterol Jpn. 1975;10:52-64. [Cited in This Article: ] |
| 62. | Pritchard DM, Przemeck SM. Review article: How useful are the rodent animal models of gastric adenocarcinoma? Aliment Pharmacol Ther. 2004;19:841-859. [Cited in This Article: ] |
| 63. | El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, Herrera J, Lissowska J, Yuan CC, Rothman N. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398-402. [Cited in This Article: ] |
| 64. | Presotto F, Sabini B, Cecchetto A, Plebani M, De Lazzari F, Pedini B, Betterle C. Helicobacter pylori infection and gastric autoimmune diseases: is there a link? Helicobacter. 2003;8:578-584. [Cited in This Article: ] |
| 65. | Stolte M, Meier E, Meining A. Cure of autoimmune gastritis by Helicobacter pylori eradication in a 21-year-old male. Z Gastroenterol. 1998;36:641-643. [Cited in This Article: ] |
| 66. | Havu N. Enterochromaffin-like cell carcinoids of gastric mucosa in rats after life-long inhibition of gastric secretion. Digestion. 1986;35 Suppl 1:42-55. [Cited in This Article: ] |
| 67. | Burkitt MD, Pritchard DM. Review article: Pathogenesis and management of gastric carcinoid tumours. Aliment Pharmacol Ther. 2006;24:1305-1320. [Cited in This Article: ] |
| 68. | Berna MJ, Annibale B, Marignani M, Luong TV, Corleto V, Pace A, Ito T, Liewehr D, Venzon DJ, Delle Fave G. A prospective study of gastric carcinoids and enterochromaffin-like cell changes in multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: identification of risk factors. J Clin Endocrinol Metab. 2008;93:1582-1591. [Cited in This Article: ] |
| 69. | Carboni M, Guadagni S, Pistoia MA, Amicucci G, Lolli D, Palumbo G, Ludovico C, Walters C, Smith P, Viti G. Chronic atrophic gastritis and risk of N-nitroso compounds carcinogenesis. Langenbecks Arch Chir. 1988;373:82-90. [Cited in This Article: ] |
| 70. | Jensen RT. Consequences of long-term proton pump blockade: insights from studies of patients with gastrinomas. Basic Clin Pharmacol Toxicol. 2006;98:4-19. [Cited in This Article: ] |
| 71. | Fujii T, Kawai T, Saito K, Hishima T, Hayashi Y, Imura J, Hironaka M, Hosoya Y, Koike M, Fukayama M. MEN1 gene mutations in sporadic neuroendocrine tumors of foregut derivation. Pathol Int. 1999;49:968-973. [Cited in This Article: ] |
| 72. | D'Adda T, Keller G, Bordi C, Höfler H. Loss of heterozygosity in 11q13-14 regions in gastric neuroendocrine tumors not associated with multiple endocrine neoplasia type 1 syndrome. Lab Invest. 1999;79:671-677. [Cited in This Article: ] |
| 73. | Higham AD, Dimaline R, Varro A, Attwood S, Armstrong G, Dockray GJ, Thompson DG. Octreotide suppression test predicts beneficial outcome from antrectomy in a patient with gastric carcinoid tumor. Gastroenterology. 1998;114:817-822. [Cited in This Article: ] |
| 74. | Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988;48:3554-3560. [Cited in This Article: ] |
| 75. | McGuigan JE, Trudeau WL. Serum and tissue gastrin concentrations in patients with carcinoma of the stomach. Gastroenterology. 1973;64:22-25. [Cited in This Article: ] |
| 76. | Rakic S, Milicevic MN. Serum gastrin levels in patients with intestinal and diffuse type of gastric cancer. Br J Cancer. 1991;64:1189. [Cited in This Article: ] |
| 77. | Soran A, Aslar AK, Cöl C. Are preoperative serum gastrin levels related to resectability and survival in gastric cancer? Int J Clin Pract. 2000;54:652-653. [Cited in This Article: ] |
| 78. | Lin JT, Lee WC, Wu MS, Wang JT, Wang TH, Chen CJ. Diagnosis of gastric adenocarcinoma using a scoring system: combined assay of serological markers of Helicobacter pylori infection, pepsinogen I and gastrin. J Gastroenterol. 1995;30:156-161. [Cited in This Article: ] |
| 79. | Storskrubb T, Aro P, Ronkainen J, Sipponen P, Nyhlin H, Talley NJ, Nyhlin H, Engstrand L, Stolte M, Vieth M, Walker M, Agréus L. Serum biomarkers provide an accurate method for diagnosis of atrophic gastritis in a general population: The Kalixanda study. Scand J Gastroenterol. 2008;43:1448-1455. [Cited in This Article: ] |
| 80. | Hansen S, Vollset SE, Derakhshan MH, Fyfe V, Melby KK, Aase S, Jellum E, McColl KE. Two distinct aetiologies of cardia cancer; evidence from premorbid serological markers of gastric atrophy and Helicobacter pylori status. Gut. 2007;56:918-925. [Cited in This Article: ] |
| 81. | Koivusalo AI, Pakarinen MP, Kolho KL. Is GastroPanel serum assay useful in the diagnosis of Helicobacter pylori infection and associated gastritis in children? Diagn Microbiol Infect Dis. 2007;57:35-38. [Cited in This Article: ] |
| 82. | Henwood M, Clarke PA, Smith AM, Watson SA. Expression of gastrin in developing gastric adenocarcinoma. Br J Surg. 2001;88:564-568. [Cited in This Article: ] |
| 83. | Hur K, Kwak MK, Lee HJ, Park DJ, Lee HK, Lee HS, Kim WH, Michaeli D, Yang HK. Expression of gastrin and its receptor in human gastric cancer tissues. J Cancer Res Clin Oncol. 2006;132:85-91. [Cited in This Article: ] |
| 84. | Stephens MR, Hopper AN, Lewis WG, Blackshaw G, Edwards P, Osborne B, Thompson IW. Prognostic significance of gastrin expression in patients undergoing R0 gastrectomy for adenocarcinoma. Gastric Cancer. 2007;10:159-166. [Cited in This Article: ] |
| 85. | Harrison JD, Jones JA, Morris DL. The effect of the gastrin receptor antagonist proglumide on survival in gastric carcinoma. Cancer. 1990;66:1449-1452. [Cited in This Article: ] |
| 86. | Watson SA, Michaeli D, Grimes S, Morris TM, Robinson G, Varro A, Justin TA, Hardcastle JD. Gastrimmune raises antibodies that neutralize amidated and glycine-extended gastrin-17 and inhibit the growth of colon cancer. Cancer Res. 1996;56:880-885. [Cited in This Article: ] |
| 87. | Watson SA, Morris TM, Varro A, Michaeli D, Smith AM. A comparison of the therapeutic effectiveness of gastrin neutralisation in two human gastric cancer models: relation to endocrine and autocrine/paracrine gastrin mediated growth. Gut. 1999;45:812-817. [Cited in This Article: ] |
| 88. | Gilliam AD, Watson SA, Henwood M, McKenzie AJ, Humphreys JE, Elder J, Iftikhar SY, Welch N, Fielding J, Broome P. A phase II study of G17DT in gastric carcinoma. Eur J Surg Oncol. 2004;30:536-543. [Cited in This Article: ] |
| 89. | Ajani JA, Randolph Hecht J, Ho L, Baker J, Oortgiesen M, Eduljee A, Michaeli D. An open-label, multinational, multicenter study of G17DT vaccination combined with cisplatin and 5-fluorouracil in patients with untreated, advanced gastric or gastroesophageal cancer: the GC4 study. Cancer. 2006;106:1908-1916. [Cited in This Article: ] |
| 90. | Konturek PC, Konturek SJ, Starzyska T, Marlicz K, Bielanski W, Pierzchalski P, Karczewska E, Hartwich A, Rembiasz K, Lawniczak M. Helicobacter pylori-gastrin link in MALT lymphoma. Aliment Pharmacol Ther. 2000;14:1311-1318. [Cited in This Article: ] |
| 91. | Ohashi S, Segawa K, Okamura S, Urano F, Kanamori S, Hosoi T, Ishikawa H, Kanamori A, Kitabatake S, Sano H. Gastrin and Helicobacter pylori in low-grade MALT lymphoma patients. Scand J Gastroenterol. 2002;37:279-286. [Cited in This Article: ] |
| 92. | Abraham SC, Nobukawa B, Giardiello FM, Hamilton SR, Wu TT. Sporadic fundic gland polyps: common gastric polyps arising through activating mutations in the beta-catenin gene. Am J Pathol. 2001;158:1005-1010. [Cited in This Article: ] |
| 93. | Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, Church JM. Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin Gastroenterol Hepatol. 2008;6:180-185. [Cited in This Article: ] |
| 94. | Attard TM, Cuffari C, Tajouri T, Stoner JA, Eisenberg MT, Yardley JH, Abraham SC, Perry D, Vanderhoof J, Lynch H. Multicenter experience with upper gastrointestinal polyps in pediatric patients with familial adenomatous polyposis. Am J Gastroenterol. 2004;99:681-686. [Cited in This Article: ] |
| 95. | Jalving M, Koornstra JJ, Götz JM, van der Waaij LA, de Jong S, Zwart N, Karrenbeld A, Kleibeuker JH. High-grade dysplasia in sporadic fundic gland polyps: a case report and review of the literature. Eur J Gastroenterol Hepatol. 2003;15:1229-1233. [Cited in This Article: ] |
| 96. | Jalving M, Koornstra JJ, Boersma-van Ek W, de Jong S, Karrenbeld A, Hollema H, de Vries EG, Kleibeuker JH. Dysplasia in fundic gland polyps is associated with nuclear beta-catenin expression and relatively high cell turnover rates. Scand J Gastroenterol. 2003;38:916-922. [Cited in This Article: ] |
| 97. | Abraham SC, Park SJ, Mugartegui L, Hamilton SR, Wu TT. Sporadic fundic gland polyps with epithelial dysplasia: evidence for preferential targeting for mutations in the adenomatous polyposis coli gene. Am J Pathol. 2002;161:1735-1742. [Cited in This Article: ] |
| 98. | Kuipers EJ. Proton pump inhibitors and gastric neoplasia. Gut. 2006;55:1217-1221. [Cited in This Article: ] |
| 99. | Fossmark R, Jianu CS, Martinsen TC, Qvigstad G, Syversen U, Waldum HL. Serum gastrin and chromogranin A levels in patients with fundic gland polyps caused by long-term proton-pump inhibition. Scand J Gastroenterol. 2007;55:1-5. [Cited in This Article: ] |
| 100. | Yeomans ND, Dent J. Personal review: alarmism or legitimate concerns about long-term suppression of gastric acid secretion? Aliment Pharmacol Ther. 2000;14:267-271. [Cited in This Article: ] |
| 101. | Waldum HL, Brenna E. Personal review: is profound acid inhibition safe? Aliment Pharmacol Ther. 2000;14:15-22. [Cited in This Article: ] |
| 102. | Coté GA, Howden CW. Potential adverse effects of proton pump inhibitors. Curr Gastroenterol Rep. 2008;10:208-214. [Cited in This Article: ] |
| 103. | Lou HY, Chang CC, Sheu MT, Chen YC, Ho HO. Optimal dose regimens of esomeprazole for gastric acid suppression with minimal influence of the CYP2C19 polymorphism. Eur J Clin Pharmacol. 2008;10. [Cited in This Article: ] |
| 104. | Klinkenberg-Knol EC, Nelis F, Dent J, Snel P, Mitchell B, Prichard P, Lloyd D, Havu N, Frame MH, Romàn J. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661-669. [Cited in This Article: ] |
| 105. | Hirschowitz BI, Worthington J, Mohnen J. Vitamin B12 deficiency in hypersecretors during long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther. 2008;27:1110-1121. [Cited in This Article: ] |
| 106. | Ruscin JM, Page RL 2nd, Valuck RJ. Vitamin B(12) deficiency associated with histamine(2)-receptor antagonists and a proton-pump inhibitor. Ann Pharmacother. 2002;36:812-816. [Cited in This Article: ] |
| 107. | Hutchinson C, Geissler CA, Powell JJ, Bomford A. Proton pump inhibitors suppress absorption of dietary non-haem iron in hereditary haemochromatosis. Gut. 2007;56:1291-1295. [Cited in This Article: ] |
| 108. | Kaur S, Vaishnavi C, Prasad KK, Ray P, Kochhar R. Comparative role of antibiotic and proton pump inhibitor in experimental Clostridium difficile infection in mice. Microbiol Immunol. 2007;51:1209-1214. [Cited in This Article: ] |
| 109. | Jayatilaka S, Shakov R, Eddi R, Bakaj G, Baddoura WJ, DeBari VA. Clostridium difficile infection in an urban medical center: five-year analysis of infection rates among adult admissions and association with the use of proton pump inhibitors. Ann Clin Lab Sci. 2007;37:241-247. [Cited in This Article: ] |
| 110. | Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102:2047-2056; quiz 2057. [Cited in This Article: ] |
| 111. | O'Connell MB, Madden DM, Murray AM, Heaney RP, Kerzner LJ. Effects of proton pump inhibitors on calcium carbonate absorption in women: a randomized crossover trial. Am J Med. 2005;118:778-781. [Cited in This Article: ] |
| 112. | Cui GL, Syversen U, Zhao CM, Chen D, Waldum HL. Long-term omeprazole treatment suppresses body weight gain and bone mineralization in young male rats. Scand J Gastroenterol. 2001;36:1011-1015. [Cited in This Article: ] |
| 113. | Ottewell PD, Watson AJ, Wang TC, Varro A, Dockray GJ, Pritchard DM. Progastrin stimulates murine colonic epithelial mitosis after DNA damage. Gastroenterology. 2003;124:1348-1357. [Cited in This Article: ] |
| 114. | Singh P, Velasco M, Given R, Varro A, Wang TC. Progastrin expression predisposes mice to colon carcinomas and adenomas in response to a chemical carcinogen. Gastroenterology. 2000;119:162-171. [Cited in This Article: ] |
| 115. | Cobb S, Wood T, Tessarollo L, Velasco M, Given R, Varro A, Tarasova N, Singh P. Deletion of functional gastrin gene markedly increases colon carcinogenesis in response to azoxymethane in mice. Gastroenterology. 2002;123:516-530. [Cited in This Article: ] |
| 116. | Rünkorg K, Veraksits A, Kurrikoff K, Luuk H, Raud S, Abramov U, Matsui T, Bourin M, Kõks S, Vasar E. Distinct changes in the behavioural effects of morphine and naloxone in CCK2 receptor-deficient mice. Behav Brain Res. 2003;144:125-135. [Cited in This Article: ] |
| 117. | Abramov U, Raud S, Innos J, Kõks S, Matsui T, Vasar E. Gender specific effects of ethanol in mice, lacking CCK2 receptors. Behav Brain Res. 2006;175:149-156. [Cited in This Article: ] |
| 118. | Rünkorg K, Veraksits A, Kurrikoff K, Luuk H, Raud S, Abramov U, Matsui T, Bourin M, Kõks S, Vasar E. Distinct changes in the behavioural effects of morphine and naloxone in CCK2 receptor-deficient mice. Behav Brain Res. 2003;144:125-135. [Cited in This Article: ] |
| 119. | Abramov U, Raud S, Kõks S, Innos J, Kurrikoff K, Matsui T, Vasar E. Targeted mutation of CCK(2) receptor gene antagonises behavioural changes induced by social isolation in female, but not in male mice. Behav Brain Res. 2004;155:1-11. [Cited in This Article: ] |
| 120. | Raud S, Innos J, Abramov U, Reimets A, Kõks S, Soosaar A, Matsui T, Vasar E. Targeted invalidation of CCK2 receptor gene induces anxiolytic-like action in light-dark exploration, but not in fear conditioning test. Psychopharmacology (Berl). 2005;181:347-357. [Cited in This Article: ] |