Abstract
Introduction
The aim of therapeutic regimens using proton pump inhibitors (PPIs) in patients with acid-related diseases is to potently inhibit acid secretion for the full 24 h. However, optimum treatment is still unclear because the pharmacodynamics of PPIs differ among CYP2C19 genotypes and most of the previous studies have had loss of sample power.
Methods
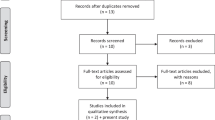
Using pH monitoring, we compared acid inhibition at standard dosage of omeprazole (20 mg, 50 times), lansoprazole (30 mg, 68 times), and rabeprazole (10 mg, 65 times) in Helicobacter pylori-negative healthy young Japanese volunteers.
Results
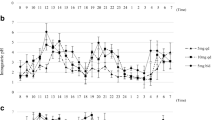
Median pH with rabeprazole was 5.4 (3.3–7.5), which was significantly greater than with either omeprazole [4.4 (2.1–7.3)] or lansoprazole [4.8 (3.5–6.4)] (both P < 0.05). Median 24-h pH differed among the different CYP2C19 genotypes in all three PPIs. In CYP2C19 extensive metabolizers (EMs), the genotype that is refractory to PPI treatment, median pH with omeprazole, lansoprazole, and rabeprazole was 3.8 (2.1–4.4), 4.5 (3.5–5.3) and 4.8 (3.3–7.5), respectively.
Discussion
Treatment with the selected PPIs at their standard dosages had difficulty maintaining acid inhibition for a full 24 h, especially in CYP2C19 EM. However, rabeprazole has the merit of less influence of CYP2C19 genotype compared with the other PPIs.


Similar content being viewed by others
Abbreviations
- CYP2C19:
-
S-mephenytoin 4′-hydroxylase
- EM:
-
Extensive metabolizer
- IM:
-
Intermediate metabolizer
- PPI:
-
Proton pump inhibitor
- PM:
-
Poor metabolizer
References
Barer D, Ogilvie A, Henry D et al (1983) Cimetidine and tranexamic acid in the treatment of acute upper-gastrointestinal-tract bleeding. N Engl J Med 308:1571–1575
Bell NJ, Burget D, Howden CW et al (1992) Appropriate acid suppression for the management of gastro-oesophageal reflux disease. Digestion 51(Suppl 1):59–67
Sugimoto M, Nishino M, Kodaira C et al (2011) Impact of acid inhibition on esophageal mucosal injury induced by low-dose aspirin. Digestion 85:9–17. doi:10.1159/000329295
Walsh JH, Peterson WL (1995) The treatment of Helicobacter pylori infection in the management of peptic ulcer disease. N Engl J Med 333:984–991
Furuta T, Sagehashi Y, Shirai N et al (2005) Influence of CYP2C19 polymorphism and Helicobacter pylori genotype determined from gastric tissue samples on response to triple therapy for H pylori infection. Clin Gastroenterol Hepatol 3:564–573
Furuta T, Shirai N, Watanabe F et al (2002) Effect of cytochrome P4502C19 genotypic differences on cure rates for gastroesophageal reflux disease by lansoprazole. Clin Pharmacol Ther 72:453–460
Sugimoto M, Furuta T, Shirai N et al (2007) Evidence that the degree and duration of acid suppression are related to Helicobacter pylori eradication by triple therapy. Helicobacter 12:317–323
Ishizaki T, Horai Y (1999) Review article: cytochrome P450 and the metabolism of proton pump inhibitors—emphasis on rabeprazole. Aliment Pharmacol Ther 13(Suppl 3):27–36
Horai Y, Kimura M, Furuie H et al (2001) Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther 15:793–803
Shirai N, Furuta T, Moriyama Y et al (2001) Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther 15:1929–1937
Shirai N, Furuta T, Xiao F et al (2002) Comparison of lansoprazole and famotidine for gastric acid inhibition during the daytime and night-time in different CYP2C19 genotype groups. Aliment Pharmacol Ther 16:837–846
Sugimoto M, Furuta T, Shirai N et al (2004) Different dosage regimens of rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotype status. Clin Pharmacol Ther 76:290–301
Chang M, Dahl ML, Tybring G et al (1995) Use of omeprazole as a probe drug for CYP2C19 phenotype in Swedish Caucasians: comparison with S-mephenytoin hydroxylation phenotype and CYP2C19 genotype. Pharmacogenetics 5:358–363
Kubota T, Chiba K, Ishizaki T (1996) Genotyping of S-mephenytoin 4′-hydroxylation in an extended Japanese population. Clin Pharmacol Ther 60:661–666
Furuta T, Ohashi K, Kosuge K et al (1999) CYP2C19 genotype status and effect of omeprazole on intragastric pH in humans. Clin Pharmacol Ther 65:552–561
Furuta T, Shirai N, Takashima M et al (2001) Effects of genotypic differences in CYP2C19 status on cure rates for Helicobacter pylori infection by dual therapy with rabeprazole plus amoxicillin. Pharmacogenetics 11:341–348
Sugimoto M, Furuta T, Shirai N et al (2005) Comparison of an increased dosage regimen of rabeprazole versus a concomitant dosage regimen of famotidine with rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotypes. Clin Pharmacol Ther 77:302–311
Hatlebakk JG, Katz PO, Castell DO (1999) Medical therapy. Management of the refractory patient. Gastroenterol Clin N Am 28:847–860
Joh T, Miwa H, Higuchi K et al (2007) Validity of endoscopic classification of nonerosive reflux disease. J Gastroenterol 42:444–449
Miwa H, Sasaki M, Furuta T et al (2007) Efficacy of rabeprazole on heartburn symptom resolution in patients with non-erosive and erosive gastro-oesophageal reflux disease: a multicenter study from Japan. Aliment Pharmacol Ther 26:69–77
Sugimoto M, Nishino M, Kodaira C et al (2011) Characteristics of non-erosive gastroesophageal reflux disease refractory to proton pump inhibitor therapy. World J Gastroenterol 17:1858–1865. doi:10.3748/wjg.v17.i14.1858
Klinkenberg-Knol EC, Festen HP, Jansen JB et al (1994) Long-term treatment with omeprazole for refractory reflux esophagitis: efficacy and safety. Ann Intern Med 121:161–167
Peghini PL, Katz PO, Bracy NA et al (1998) Nocturnal recovery of gastric acid secretion with twice-daily dosing of proton pump inhibitors. Am J Gastroenterol 93:763–767
Hatlebakk JG, Katz PO, Kuo B et al (1998) Nocturnal gastric acidity and acid breakthrough on different regimens of omeprazole 40 mg daily. Aliment Pharmacol Ther 12:1235–1240
Katsube T, Adachi K, Kawamura A et al (2000) Helicobacter pylori infection influences nocturnal gastric acid breakthrough. Aliment Pharmacol Ther 14:1049–1056
Nishino M, Sugimoto M, Kodaira C et al (2010) Relationship between low-dose aspirin-induced gastric mucosal injury and intragastric pH in healthy volunteers. Dig Dis Sci 55:1627–1636. doi:10.1007/s10620-009-0920-3, CDAI: 19672708
Kodaira C, Sugimoto M, Nishino M et al (2009) Effect of MDR1 C3435T polymorphism on lansoprazole in healthy Japanese subjects. Eur J Clin Pharmacol 65:593–600. doi:10.1007/s00228-009-0625-8, CDAI: 19238367
Furuta T, Shirai N, Xiao F et al (2001) Effect of high-dose lansoprazole on intragastic pH in subjects who are homozygous extensive metabolizers of cytochrome P4502C19. Clin Pharmacol Ther 70:484–492, CDAI: 11719736
Furuta T, Shirai N, Kodaira M et al (2007) Pharmacogenomics-based tailored versus standard therapeutic regimen for eradication of H. pylori. Clin Pharmacol Ther 81:521–528, CDAI: 17215846
Uotani T, Sugimoto M, Nishino M et al (2012) Ability of rabeprazole to prevent gastric mucosal damage from clopidogrel and low doses of aspirin depends on CYP2C19 genotype. Clin Gastroenterol Hepatol. doi:10.1016/j.cgh.2012.04.016, CDAI: 22542748
Kurata S, Kanagawa T, Yamada K et al (2001) Fluorescent quenching-based quantitative detection of specific DNA/RNA using a BODIPY((R)) FL-labeled probe or primer. Nucleic Acids Res 29:E34, CDAI: 11239011
Torimura M, Kurata S, Yamada K et al (2001) Fluorescence-quenching phenomenon by photoinduced electron transfer between a fluorescent dye and a nucleotide base. Anal Sci Int J Jpn Soc Anal Chem 17:155–160, CDAI: 11993654
Furuta T, Soya Y, Sugimoto M et al (2013) Rapid automated genotyping of CYP2C19 and Helicobacter pylori 23S rRNA gene in gastric juice. J Gastroenterol Hepatol Res 2:506–512
De Morais SM, Wilkinson GR, Blaisdell J et al (1994) Identification of a new genetic defect responsible for the polymorphism of (S)-mephenytoin metabolism in Japanese. Mol Pharmacol 46:594–598, CDAI: 7969038
Adachi K, Fujishiro H, Katsube T et al (2001) Predominant nocturnal acid reflux in patients with Los Angeles grade C and D reflux esophagitis. J Gastroenterol Hepatol 16:1191–1196, CDAI: 11903734
Yasuda S, Horai Y, Tomono Y et al (1995) Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′-hydroxylation status. Clin Pharmacol Ther 58:143–154, CDAI: 7648764
Kawamura M, Ohara S, Koike T et al (2003) The effects of lansoprazole on erosive reflux oesophagitis are influenced by CYP2C19 polymorphism. Aliment Pharmacol Ther 17:965–973, CDAI: 12656699
Kawamura M, Ohara S, Koike T et al (2007) Cytochrome P450 2C19 polymorphism influences the preventive effect of lansoprazole on the recurrence of erosive reflux esophagitis. J Gastroenterol Hepatol 22:222–226. doi:10.1111/j.1440-1746.2006.04419.x, CDAI: 17295875
Sim SC, Risinger C, Dahl ML et al (2006) A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther 79:103–113, CDAI: 16413245
Sugimoto K, Uno T, Yamazaki H et al (2008) Limited frequency of the CYP2C19*17 allele and its minor role in a Japanese population. Br J Clin Pharmacol 65:437–439. doi:10.1111/j.1365-2125.2007.03057.x, CDAI: 2291245
Kinoshita Y, Hongo M (2012) Efficacy of twice-daily rabeprazole for reflux esophagitis patients refractory to standard once-daily administration of PPI: the Japan-based TWICE study. Am J Gastroenterol 107:522–530. doi:10.1038/ajg.2012.19, CDAI: 22433921
Sugimoto M, Shirai N, Nishino M et al (2012) Rabeprazole 10 mg q.d.s. decreases 24-h intragastric acidity significantly more than rabeprazole 20 mg b.d. or 40 mg o.m., overcoming CYP2C19 genotype. Aliment Pharmacol Ther 36:627–634. doi:10.1111/apt.12014, CDAI: 22882464
Acknowledgments
This study was supported by a grant-in-aid from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (22790640 and 24590912).
Conflicts of interest
None of the authors has any conflict of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugimoto, M., Shirai, N., Nishino, M. et al. Comparison of acid inhibition with standard dosages of proton pump inhibitors in relation to CYP2C19 genotype in Japanese. Eur J Clin Pharmacol 70, 1073–1078 (2014). https://doi.org/10.1007/s00228-014-1713-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-014-1713-y