Abstract
Background:
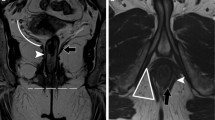
Successful surgery for perianal fistula is contingent upon accurate pre-operative classification of the primary tract and its extensions. We aimed to find, using “evidence based medicine” (EBM) methods, the optimal technique for fistula classification: MRI, anal endosonography (AES) or clinical examination.
Methods:
A clinical question was derived, “In patients suspected of having perianal fistula, how does MRI compare to AES and clinical assessment for discriminating simple from complex disease”. A search of primary literature and secondary evidence resources was performed and expert opinion sought. Inclusion criteria were blinded prospective studies (level 2b +) of patients undergoing preoperative MRI, clinical examination ± AES using a clinical outcome based reference standard. Retrieved literature was appraised using EBM methods.
Results:
The highest-ranking evidence found was level 1b. MRI is more sensitive 0.97(CI 0.92–1.01) than clinical examination, 0.75(0.65–0.86) but comparable to AES, 0.92(0.85–0.99) for discriminating complex from simple disease. The positive LR for MRI confirming complex disease is 22.7 compared to 2.1 and 6.2 for clinical examination and AES, respectively.
Conclusion:
MRI is the optimal technique for discriminating complex from simple perianal fistula, although AES is superior to clinical examination, and may be used if MRI availability is restricted.




Similar content being viewed by others
References
Staunton M. Evidence-based radiology: steps 1 and 2––asking answerable questions and searching for evidence. Radiology 2007; 242: 23–31
http://www.clinicalevidence.com/ceweb/index.jsp Accessed 16th April 2007
http://www.cochrane.org Accessed 16th April 2007
http://www.tripdatabase.com Accessed 18th April 2007
http://www.guideline.gov Accessed 18th April 2007
Huprich JE, Bree RL, Foley WD, Gay SB, Glick SN, Heiken JP, Levine MS, Ros PR, Rosen MP, Shuman WP, Greene FL, Rockey DC, Expert panel on gastrointestinal imaging. imaging recommendations for patients with Crohn’s disease. [online publication]. Reston (VA): American College of Radiology (ACR); 2005. p 11 [46 references]
American Gastroenterological Association Clinical Practice Committee 2003 American Gastroenterological Association medical position statement: perianal Crohn’s disease. Gastroenterology 125:1503–1507
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=8585&string=. Accessed 18th April 2007
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=4582&string=. Accessed 18th April 2007
Halligan S, Altman DG. Evidence-based practice in radiology: steps 3 and 4––appraise and apply systematic reviews and meta-analyses. Radiology 2007; 243: 13–27
Chapple KS, Spencer JA, Windsor ACJ, Wilson D, Ward J, Ambrose NS 2000 Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum; 43:511–516
Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CRG 2004 Clinical examination, endosonography, and mr imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology; 233:674–681
Dodd JJ 2007 Evidence-based practice in radiology: steps 3 and 4––appraise and apply diagnostic radiology literature. Radiology 242: 342–354
http://www.cebm.net/levels_of_evidence.asp. Accessed 18th April 2007
http://www.ebr.ie/spreadsheets/diagnostic.xls. Accessed 18th April 2007
Mahjoubi B, Haizadch Kharazi H, Mirzaei R, Moghimi A, Changizi A 2005 Diagnostic accuracy of body coil MRI in describing the characteristics of perianal fistulas. Colorectal Dis 8:202–207
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC 2003 Standards for reporting of diagnostic accuracy. towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Clin Radiol; 58:575–580
Acknowledgments
The authors would like to thank Professor Clive Bartram for his expert opinion and valuable contribution to our review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahni, V.A., Ahmad, R. & Burling, D. Which method is best for imaging of perianal fistula?. Abdom Imaging 33, 26–30 (2008). https://doi.org/10.1007/s00261-007-9309-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9309-y