Abstract
Background
Immunochemical tests show important advantages over chemical-based faecal occult blood tests (FOBT) for colorectal cancer (CRC) screening, but comparison studies are limited. This study was performed to compare the accuracy of a sensitive immunochemical test with the guaiac test for detecting significant neoplasia (advanced adenomas and CRC) in an average-risk population.
Methods
A random sample of 2288 asymptomatic subjects 50–79 years of age was prospectively included. Participants received three cards of the guaiac test, one sample of a latex-agglutination test (haemoglobin cut-off 50 ng/ml), and an invitation to undergo colonoscopy. Test sensitivity, specificity, and positive and negative predictive values (PPV and NPV) were calculated in 1756 compliers.
Results
Immunochemical and guaiac tests were positive in 143 (8.1%) and 62 (3.5%) subjects, respectively. Complete colonoscopy, performed in 402 participants (158 FOBT+ and 244 FOBT−), detected 14 (0.8%) patients with CRC and 49 (2.8%) with advanced adenomas. The immunochemical and guaiac tests for significant colorectal neoplasia showed sensitivities of 61% versus 23.8%, specificities of 95.1% versus 97.7%, PPVs of 43.4% versus 39.0%, and NPVs of 97.5% versus 95.4%, respectively. Proximal significant neoplasms were more frequently detected with the immunochemical test (85% vs. 15%) The relative risk for detecting significant neoplasia was superior in patients with a positive immunochemical test (RR 16.93; CI 7.94–36.10) than with a positive guaiac test (RR 3.34; CI 2.17–5.15).
Conclusion
A sensitive immunochemical test is markedly superior to the guaiac test for detecting significant colorectal neoplasia, and should be considered the first-choice FOBT for CRC screening in the average-risk population.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is globally the most frequent cancer and the second leading cause of cancer-related mortality in Europe [1]. Standard guaiac faecal occult blood tests (G-FOBT) have shown a reduction in CRC mortality [2–5] and incidence [6] in randomized trials. In spite of their proven efficacy, several major flaws such as a less than modest sensitivity for significant neoplasia and the need for a previous diet have prompted the search for more efficient non-invasive CRC screening methods. Faecal immunochemical tests can specifically detect human globin and are especially sensitive to colorectal but not upper gastrointestinal bleeding [7]. Moreover, an increased sensitivity for faecal blood detection compared to G-FOBT allows for a theoretical increase in colorectal neoplasia diagnostic power. However, early immunochemical tests rarely showed a substantially improved performance compared to G-FOBT [8]. Although those tests detected lower levels of faecal haemoglobin (200–300 μg Hb/g faeces) than G-FOBT (750 μg Hb/g faeces), their sensitivity was still low compared to currently available highly sensitive faecal immunochemical tests (up to 10 μg Hb/g faeces) [9–12].
When they used a rehydrated G-FOBT (Hemoccult®), the Minnesota study [6] reported reductions of 20 and 17% in CRC incidence for annually and biennially screened subjects, respectively, after an 18-year follow-up. It has been suggested that faecal immunochemical tests may reduce the risk of developing CRC by 28–46% due to a high sensitivity for detecting advanced adenomas (≥10 mm in size, >20% villous architecture, or presence of high-grade dysplasia) [13]. The detection rate of these lesions has been reported to be as high as 50–71% when using immunochemical tests, as compared to 10–31% when using standard G-FOBT [12, 14, 15]. However, there are few average-risk population-based prospective studies [9, 16–20] that have compared G-FOBT and highly-sensitive faecal immunochemical tests for the detection of CRC and advanced adenomas.
The aim of the current study was to compare the diagnostic accuracy of a highly sensitive (threshold detection rate of 50 ng/ml buffer) latex-agglutination faecal occult blood test (LA-FOBT) with G-FOBT for detecting significant colorectal neoplasia (advanced adenoma or CRC) in the average-risk population.
Methods
Study population and design
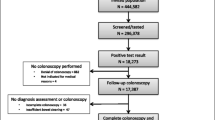
From January 2004 to August 2006, 3092 subjects (1062 males, 2030 females) were randomly selected (stratifying by age and sex) from among 71673 inhabitants aged 50–79 years in the north area of Tenerife, Spain. Among them, 804 (25.6%) were excluded for different reasons (Fig. 1). Therefore, 2288 (74%) subjects were finally included.
All participants received two sets of FOBT kits for sampling: three cards of a non-rehydrated G-FOBT (Hemofec™, Roche Diagnostics S.L., Barcelona, Spain), which has a detection limit of ~750 μg Hb/g faeces, and a single sample of a qualitative LA-FOBT (OC-Light™, Eiken Chemical Co., Ltd., Japan) that specifically detects human haemoglobin with a sensitivity of 50 ng/ml buffer. In addition, all participants were invited to undergo colonoscopy.
The institutional review board approved the study, which is consistent with the principles of the Declaration of Helsinki, and participants gave written informed consent.
Faecal occult blood tests
Oral information was given regarding the procedures for stool sampling and storage. In addition, all participants received an explanatory flyer with drawings that detailed the procedure to be followed in order to complete both FOBT kits. Participants followed a diet without red meat, vegetables and vitamin C for 3 days before stool sampling. Individuals treated with aspirin or non-steroidal anti-inflammatory drugs during the week before randomization were excluded from the study. Faecal material for the G-FOBT was assessed from two samples taken from each of three stools. Tests with at least one positive oval out of six were considered positive.
The LA-FOBT sample was taken from the same bowel movement as the last sample for the G-FOBT. This test consists of a small tube containing buffer solution and two caps. The green cap has a small stick that is unscrewed, detached and inserted into the faeces at 6 points up to its middle portion. After that, the stick is reinserted into the tube and the cap is screwed on. Participants were asked to keep the samples in the refrigerator and return them within 3 days after sampling. Three trained investigators (AZGG, APB and MCP) who were unaware of the result of the other test developed the G-FOBT and the LA-FOBT tests. Test development was performed according to the recommendations of the distributor in the outpatient office. When developing the LA-FOBT, the white cap is open and a reactive band is introduced into the tube. Within 5 min either a single upper blue band appears or two (upper and lower) bands appear, corresponding to a negative or a positive result, respectively. Whenever only a lower band is seen or no band is present, the result is considered to be indeterminate.
Colonoscopy
Bowel cleansing for colonoscopy was performed as previously described [21]. Sedation with intravenous fentanyl and/or midazolam was offered to all subjects. Examinations were performed by 4 experienced staff endoscopists. Chromoendoscopy with indigo carmine stain (0.2–0.5%) and tattooing with Indian ink was applied when required [22]. The size of each polyp was estimated using open-biopsy forceps, which are 7 mm in diameter. Patients in whom colonoscopy did not reach the caecum because of causes other than neoplastic stricture were excluded from the analysis (Fig. 1). Endoscopists were blinded to the G-FOBT and LA-FOBT results.
Histology
Polyps sampled or removed endoscopically were submitted to standard histological examination. Following histopathological diagnosis, polyps were classified as non-neoplastic or neoplastic (adenomatous). Adenomas ≥10 mm in size, with >20% villous architecture, or harbouring high-grade dysplasia were classified as advanced adenomas. Invasive cancer was considered when malignant cells were observed beyond the muscularis mucosa. For the analysis of neoplasia detection and FOBT performance, only the most advanced lesion was considered whenever different categories of neoplastic lesions were detected in the same patient. The presence of any neoplastic lesion was considered a positive finding of colonoscopy. Significant colorectal neoplasia was defined as advanced adenoma or invasive cancer.
Follow-up
Subjects who underwent colonoscopy entered a follow-up scheme according to accepted guidelines. Subjects with a negative FOBT who refused colonoscopy entered a biennial LA-FOBT screening programme, and were contacted by telephone 2 years after having the initial screening test. They were asked about intercurrent illness or any colorectal diagnostic test performed in the interim. Individuals with positive FOBT results who refused colonoscopy were also contacted. Colonoscopy and pathology reports of examinations performed during the follow-up period were recorded.
Statistical analysis
The following variables regarding FOBT performance were recorded: positivity rate for each test, negative predictive value (NPV), and positive predictive value (PPV). Since the presence of selection bias was apparent due to the “gold standard rejection” phenomenon, the estimates of sensitivity and specificity were corrected using the method proposed by Diamond [23], which has been used in other medical settings, and even to assess other cancer screening strategies [24]. This method assumes that the disease prevalences in the positive test unverified group and the negative test unverified group are the same as those in the corresponding verified groups [25]. The adjusted sensitivity and specificity estimates for CRC and advanced adenomas were then calculated with the following equations, which are equivalent to the ones originally published [23]:
Descriptive statistics are presented as means and corresponding standard deviations or as percentages. Significant differences between men and women for continuous variables were tested for using the Student t-test. Differences in frequency distribution were compared by Fisher’s exact test or by the chi-squared test, and differences were estimated by comparing the confidence intervals of paired tests. A P value of <0.05 was considered to be statistically significant. Multivariate logistic regression analysis was performed to identify independent predictors of significant colorectal neoplasia detection. Finally, the precisions of LA-FOBT and G-FOBT were estimated by calculating the relative risk for significant colorectal neoplasia in patients with a positive or negative test [26].
Sample size
Power was calculated assuming sensitivities of the guaiac and immunochemical FOBTs to significant neoplasia of 32 and 67%, respectively [14]. Considering a prevalence of 8% for significant neoplasia in the average-risk population, an alpha risk of 0.05 and a power of 0.80, we needed to perform 313 colonoscopies to detect 25 significant lesions and to find statistically significant differences in the sensitivities of guaiac and immunochemical fecal occult blood tests.
Results
Demographic characteristics and data on FOBT and colonoscopy are shown in Table 1.
FOBT data
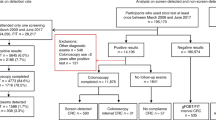
3092 persons were invited to participate in the study. Both FOBTs were returned by 1756 (76.7%), and there was a significantly higher percentage of compliant women when compared to men (78.4% vs. 73.2%, p = 0.003). There was no age difference between compliers and non-compliers (62.7 ± 7.3 years vs. 62.4 ± 7.7 years, p = 0.42), and compliance with FOBT testing did not differ significantly among the three age groups (p = 0.11). Samples were correctly prepared in 1716/1756 (97.7%) for LA-FOBT and in 1689/1756 (96.2%) for G-FOBT (p < 0.001). Samples were incorrect for both tests in 7 cases.
There was a positive result for the FOBT in 174/1756 compliers (9.9%); only the LA-FOBT was positive in 112 (6.4%), only the G-FOBT in 31 (1.8%), and both were positive in 31 (1.8%). A positive test was more frequent among males (13.4% vs. 8.3%, p = 0.01).
Colonoscopic findings
Colonoscopy was performed on 420 (23.9%) subjects. In 402 cases (95.7%) it was complete to the caecum. Of these, 158 (39.3%) and 244 (60.7%) corresponded to positive and negative FOBT cases, respectively. Altogether, 93.7% of the positive result cases (163 of the 174 positive FOBT participants) and 16.2% of the negatives (256 of 1582 the negative FOBT participants) underwent colonoscopy. Significantly more males than females underwent colonoscopy for a positive FOBT (45.5% vs. 35.5%; p = 0.042). Three males and 8 females with a positive FOBT rejected colonoscopy.
Neoplastic lesions were diagnosed in 107/158 (67.7%) subjects with positive tests and in 63/244 (25.8%) with negative results (p < 0.001). In males vs females, non-advanced adenomas were detected in 32.5% versus 23.1% (p = 0.04), advanced adenomas in 17.2% versus 9.2% (p = 0.017), and CRC in 6.6% versus 1.6% (p = 0.008), respectively. Detection of non-advanced adenomas did not differ significantly (p = 0.23) between patients with a positive LA-FOBT (43 out of 129, 33.3%) and those with a negative LA-FOBT (65 out of 273, 23.8%).
Colonoscopic findings are summarized in Table 2 in relation to the LA-FOBT or G-FOBT results. With regard to advanced adenoma and CRC, the result of the LA-FOBT was positive in 85.7 and 100%, respectively, as compared to 30.6 and 57.1% with the G-FOBT. The most significant lesion was CRC in 14 patients, advanced adenoma in 49, and non-advanced adenoma in 108. Details regarding the locations of significant neoplasms and test results are indicated in Table 3. LA-FOBT detected most significant neoplasms located either proximally (85%) or distally (91.7%) to the splenic flexure, whereas the performance of the G-FOBT was markedly lower for detecting proximal (15%) or distal (38.9%) neoplasms.
FOBT performance
The intention-to-screen detection rates for advanced adenoma and CRC were markedly superior for the LA-FOBT compared to those for the G-FOBT. Among the 2288 persons who were invited to be screened, advanced adenomas were found in 42 (1.8%; 95% CI: 1.3–2.3) with a positive LA-FOBT and in 15 (0.6%; CI: 0.3–0.9) with a positive G-FOBT (p < 0.001). In addition, CRC was found in 14 (0.6%; CI: 0.3–0.9) patients with a positive LA-FOBT and in 8 (0.3%; CI: 0.1–0.5) with a positive G-FOBT (p = 0.29). Overall, the detection rate of significant colorectal neoplasia was significantly higher (p < 0.001) among patients with a positive LA-FOBT (2.4%; CI: 1.8–3.0) than in those with a positive G-FOBT (1.0%; CI: 0.6–1.4).
The efficacies of LA-FOBT and G-FOBT as screening strategies for colorectal neoplasia detection are shown in Table 4. The sensitivities of LA-FOBT for detecting CRC and advanced adenoma were 100% (95% CI = 73.2–100) and 56.8% (95% CI = 41.8–70.7), respectively. These compare favorably with G-FOBT, which exhibited sensitivities of 54.2% (95% CI = 27.3–79.1) for CRC and 19.8% (95% CI = 6.7–43.4) for advanced adenomas. Ten (71.4%) of the invasive cancers were detected at an early stage of extension (T1–T2 N0 M0 of the Tumour Node Metastasis classification).
LA-FOBT showed a sensitivity for detecting significant colorectal neoplasia of 61% (95% CI = 47.8–72.9), which was about three times that of G-FOBT. However, the specificity of LA-FOBT was slightly lower (−2.6%) than for G-FOBT. In addition, LA-FOBT showed a higher PPV (+4.4%) and NPV (+2.1%) than G-FOBT (Table 4).
Among the 1756 subjects who returned both FOBTs, the advanced adenoma and CRC detection rates after a positive LA-FOBT were 2.4 and 0.8%, respectively. However, these values rose to 3.8 and 1.8%, respectively, when only males were considered. The advanced adenoma and CRC detection rates with the G-FOBT were 0.9 and 0.5%, respectively, and 1.3 and 1.5% for males.
According to intention to screen, the numbers that needed to be screened to find an advanced adenoma or CRC were 41 for LA-FOBT and 99 for G-FOBT. Finally, as compared with subjects with a negative test, those with a positive LA-FOBT had a markedly higher relative risk of having significant neoplasia (RR 16.93; 95% CI = 7.94–36.10) than patients with a positive G-FOBT (RR 3.34; 95% CI = 2.17–5.15).
Follow-up
Among the 1336 subjects who returned both FOBTs and refused to undergo colonoscopy, 1314 (98.3%) were contacted by telephone or mail, with a mean interval after inclusion of 968 ± 211 days. Among the 11 patients with positive FOBT who refused colonoscopy, 5 could be contacted by phone. The hospital records of those who could not be contacted were revised, and in no case was CRC found.
Twelve patients died at follow-up; cancer was the direct cause of death in 7, but none of these was a CRC. In 2 of the cases the reason could not be clarified.
Seventeen patients underwent an interval colonoscopy in the follow-up period. The most frequent reasons for colonoscopy were rectal bleeding (41.2%), constipation (17.6%), and abdominal pain (11.8%). A colonic neoplasm was detected in 5 cases. The most advanced lesion was non-advanced adenoma in 3, and advanced adenoma in 2.
Discussion
Annual or biennial FOBT remains one of the most widely accepted strategies for CRC screening in the average-risk population. Screening with G-FOBT has been shown to reduce CRC mortality and incidence in randomized controlled trials [2–6], but its use in population-based screening programs has been limited, mostly because of its low sensitivity, with detection rates of less than 50% for CRC and less than 15% for advanced adenomas [27]. Faecal immunochemical tests specifically detect human haemoglobin and have a lower haemoglobin detection threshold than G-FOBT, suggesting a better test performance for CRC screening. However, there are few studies that have compared the accuracy of both tests, and none of them used complete colonoscopy as the gold standard to determine test performance in participants with positive and negative FOBTs. In the present study, the diagnostic yield of a highly sensitive LA-FOBT was compared to a non-rehydrated G-FOBT in a large average-risk population using colonoscopy as the gold standard to determine test performance. The analysis was performed in a majority (90.8%) of patients with a positive FOBT and in those with a negative FOBT who accepted colonoscopy (15.4%). Among all of the lesions detected at colonoscopy, the LA-FOBT detected all cases of CRC and over half (56.8%) of the advanced adenomas, with a specificity for significant neoplasia of over 95%. The LA-FOBT performance values compare favorably to those obtained with the G-FOBT, which would detect only 54.2% CRC and less than one-fifth (19.1%) of the advanced adenomas.
Some previous studies have compared immunochemical fecal tests with G-FOBT in a screening population, but in most cases the population included was not strictly of average risk [17, 28, 29]. In others [14, 16], either the immunochemical test employed was markedly less sensitive than the LA-FOBT used in the current study, or colonoscopy was not offered to negative cases [14, 18, 20, 30–32].
Studies comparing the test performance of sensitive (haemoglobin cutoff of 50–100 ng/ml) immunochemical FOBT to that of a standard G-FOBT (non-rehydrated Hemocult II™, detection limit ~750 μg Hb/g faeces) have shown that the immunochemical tests exhibit a better performance than G-FOBT not only for CRC detection but also for advanced adenoma detection [9, 18–20]. Using a quantitative test (Magstream 1000™), Guittet et al. [9] showed that, at a haemoglobin detection threshold of >50 ng/ml, the immunochemical test detected more than twice as many advanced adenomas as Hemocult II™ without any loss in specificity. More recently, van Rossum et al. [18] compared the performance of a semiquantitative LA-FOBT (OC-sensor™) with a G-FOBT (Hemocult II™) in a randomized study. The immunochemical test detected 2.6 times as many advanced adenomas and 2.1 times as many CRCs as G-FOBT. In addition, Smith et al. [33] obtained similar results when a sensitive immunochemical test (InSure™) was compared with a more sensitive G-FOBT (Hemocult SENSA™, detection limit ~300 μg Hb/g faeces). More recently, Hol et al. [34] conducted a randomized study in an average-risk Danish population that compared LA-FOBT (OC-sensor™) with G-FOBT (Hemocult II™) and rectosigmoidoscopy. Although sigmoidoscopy achieved the highest detection rate, LA-FOBT detected twice as many advanced neoplasms as G-FOBT. The main drawback of these studies has been that performance estimates were made without gold standard endoscopic results on the test-negative subjects, which limits the “absolute sensitivity” of each test. In fact, assessing “absolute sensitivity” when comparing two FOBTs is a logistically difficult task requiring the administration of both tests and a gold standard exam, like colonoscopy. This is particularly hard to achieve in asymptomatic subjects where the prevalence of CRC is only 1–10/1000 and the acceptance rate of screening colonoscopy is less than 20% [35].
In the present study, we prospectively compared the test performances of a qualitative LA-FOBT (OC-Light™) and a non-rehydrated G-FOBT (HemoFec™) using colonoscopy as the gold standard test in a naïve average-risk population. Our results were in line with those commented on above. Interestingly, the detection rate of non-advanced adenomas (<10 mm in diameter, without a villous component or high-grade dysplasia) was similar between subjects with a positive or negative LA-FOBT. However, one-time screening with LA-FOBT detected over half of the advanced adenomas, whereas G-FOBT only detected 19.8% of these lesions. Altogether, these findings suggest that sensitive immunochemical tests are capable of detecting pathological bleeding in advanced adenomas and early CRCs, selecting patients adequately for colonoscopy.
In our study, a qualitative immunochemical FOBT was used. Although qualitative tests are easy to interpret and are convenient for opportunistic screening, they are not suitable for mass screening. By contrast, quantitative immunochemical FOBT tests are fully automated, minimizing human error during test development, ensuring reproducibility and quality control. In addition, they allow the haemoglobin threshold to be selected according to the available resources, and multiple samples may be processed at once. Therefore, quantitative immunochemical tests are now considered the FOBT of choice for population-based CRC screening. Recently, two studies have suggested that the optimal faecal haemoglobin cut-off for detecting advanced colorectal neoplasia is 75 ng/ml [19, 36].
An important issue in the success of a CRC screening campaign is participation rate. Our results are in line with those reported in the Minnesota study [4]. However, as other authors have pointed out, participation rates in mass screening campaigns used to be lower than in controlled trials [37]. In this regard, it has been suggested that encouraging general practitioners and implementing educational interventions may increase public awareness and improve participation [38].
A limitation of the present study was that only 15.8% of subjects with a negative FOBT underwent colonoscopy, compared to 93.7% of those with a positive test result. Taking into account that the prevalence of CRC in negative FOBT participants has been reported to be as low as 0.4% [31], very few CRCs could be expected in 256 negative FOBT participants. This imbalance in “gold standard” referral is known to be the source of selection bias. That is, subjects with a positive FOBT result are more likely to accept colonoscopy than those with a negative FOBT result. Thus, disease prevalence in the verified individuals differs from the intended average-risk population, with misleading sensitivity and specificity estimates being subsequently inferred for prospective average-risk screening [39]. To minimize this effect, we applied a correction method that analyzed sensitivity and specificity in terms of predictive accuracy of the test response [23]. Moreover, a mean follow-up period of 2 years in subjects with a negative FOBT who do not undergo colonoscopy should allow the detection of false negatives, at least for CRC, in a successive screening, or they should otherwise become clinically evident in the meantime [14]. In fact, only 2 patients with advanced adenomas were detected during the follow-up period, with no single CRC case.
In a recent study using sigmoidoscopy as the gold standard exam, Allison et al. [16] showed that FlexSure OBT™, an immunochemical test less sensitive than that used in the current study, exhibited substantially higher sensitivity than Hemocult-SENSA for detecting left-sided colorectal cancer. In the current study, we found that LA-FOBT was highly sensitive for detecting significant colorectal neoplasms located distal to the splenic flexure but also in the proximal part of the colon, whereas the G-FOBT had very limited detection power. In accordance with our results, Guittet et al. [20] observed that proximal advanced adenomas have bleeding amounts (mean of 71.9 ng/Hb/ml) that may be detected by sensitive immunochemical tests.
The high sensitivity for CRC detection observed in our study may be explained by the lower (50 ng/ml) haemoglobin threshold detection rate of the OC-Light™ test and the low number of CRCs detected. In fact, although all 14 CRCs detected by colonoscopy in the current study were positive in the LA-FOBT, the confidence interval ranged from 73.2 to 100% (Table 4). It must be noted that screening tests are not diagnostic tests, and that some CRCs may remain undetected with the LA-FOBT, even if it is highly sensitive. Therefore, it can be expected that further screening rounds with the LA-FOBT would detect previously unrecognized CRCs while they are still at a curable stage. However, these data are in concordance with a validation study from Levi et al. [36] that reported a sensitivity of 100% using a semiquantitative LA-FOBT (OC-sensor™) at a cut-off level of 50 ng/ml. The cost of the increase in sensitivity obtained with LA-FOBT is a reduction in specificity, which increases the chance of a false-positive test, resulting in a low-yield colonoscopy. In our study, twice as many subjects tested with the LA-FOBT were referred for a negative colonoscopy. By contrast, almost 6 times more patients with significant colorectal neoplasm were left undetected with the G-FOBT as compared with the LA-FOBT.
Colonoscopy screening in an average-risk population has shown that men have significantly higher prevalences of advanced adenoma and CRC than women [35]. This finding was corroborated following screening with the LA-FOBT in the present study, despite the fact that more women participated in the study. This is in line with the results of Rossum et al. [18] and provides further evidence of the high performance of the LA-FOBT for CRC screening.
In conclusion, the current study suggests that a highly sensitive LA-FOBT is more sensitive than the G-FOBT not only for CRC detection but also for advanced adenoma detection in both the proximal and distal parts of the colon, and that highly sensitive immunochemical methods should be recommended as the first line FOBT for the screening of CRC in the average-risk population.
References
Keighley MR. Gastrointestinal cancers in Europe. Aliment Pharmacol Ther. 2003;18(Suppl 3):7–30.
Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–7.
Kronborg O, Jorgensen OD, Fenger C, Rasmussen M. Randomized study of biennial screening with a faecal occult blood test: results after nine screening rounds. Scand J Gastroenterol. 2004;39:846–51.
Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365–71.
Faivre J, Dancourt V, Lejeune C, Tazi MA, Lamour J, Gerard D, et al. Reduction in colorectal cancer mortality by fecal occult blood screening in a French controlled study. Gastroenterology. 2004;126:1674–80.
Mandel JS, Church TR, Bond JH, Ederer F, Geisser MS, Mongin SJ, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–7.
Young GP, St John DJ, Winawer SJ, Rozen P. Choice of fecal occult blood tests for colorectal cancer screening: recommendations based on performance characteristics in population studies: a WHO (World Health Organization) and OMED (World Organization for Digestive Endoscopy) report. Am J Gastroenterol. 2002;97:2499–507.
Young GP. Screening for colorectal cancer: alternative faecal occult blood tests. Eur J Gastroenterol Hepatol. 1998;10:205–12.
Guittet L, Bouvier V, Mariotte N, Vallee JP, Arsene D, Boutreux S, et al. Comparison of a guaiac based and an immunochemical faecal occult blood test in screening for colorectal cancer in a general average risk population. Gut. 2007;56:210–4.
Hoepffner N, Shastri YM, Hanisch E, Rosch W, Mossner J, Caspary WF, et al. Comparative evaluation of a new bedside faecal occult blood test in a prospective multicentre study. Aliment Pharmacol Ther. 2006;23:145–54.
Levi Z, Rozen P, Hazazi R, Vilkin A, Wakef A, Maoz E, et al. Can quantification of faecal occult blood predetermine the need for colonoscopy in patients at risk for non-syndromic familial colorectal cancer? Aliment Pharmacol Ther. 2006;24:1475–81.
Vilkin A, Rozen P, Levi Z, Waked A, Maoz E, Birkenfeld S, et al. Performance characteristics and evaluation of an automated-developed and quantitative, immunochemical, fecal occult blood screening test. Am J Gastroenterol. 2005;100:2519–25.
Nakajima M, Saito H, Soma Y, Sobue T, Tanaka M, Munakata A. Prevention of advanced colorectal cancer by screening using the immunochemical faecal occult blood test: a case–control study. Br J Cancer. 2003;89:23–8.
Allison JE, Tekawa IS, Ransom LJ, Adrain AL. A comparison of fecal occult-blood tests for colorectal-cancer screening. N Engl J Med. 1996;334:155–9.
Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004;351:2704–14.
Allison JE, Sakoda LC, Levin TR, Tucker JP, Tekawa IS, Cuff T, et al. Screening for colorectal neoplasms with new fecal occult blood tests: update on performance characteristics. J Natl Cancer Inst. 2007;99:1462–70.
Castiglione G, Grazzini G, Ciatto S. Guaiac and immunochemical tests for faecal occult blood in colorectal cancer screening. Br J Cancer. 1992;65:942–4.
van Rossum LG, van Rijn AF, Laheij RJ, van Oijen MG, Fockens P, van Krieken HH, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135:82–90.
Hol L, Wilschut JA, van Ballegooijen M, van Vuuren AJ, van der Valk H, Reijerink JC, et al. Screening for colorectal cancer: random comparison of guaiac and immunochemical faecal occult blood testing at different cut-off levels. Br J Cancer. 2009;100:1103–10.
Guittet L, Bouvier V, Mariotte N, Vallee JP, Levillain R, Tichet J, et al. Comparison of a guaiac and an immunochemical faecal occult blood test for the detection of colonic lesions according to lesion type and location. Br J Cancer. 2009;100:1230–5.
Parra-Blanco A, Nicolas-Perez D, Gimeno-Garcia A, Grosso B, Jimenez A, Ortega J, et al. The timing of bowel preparation before colonoscopy determines the quality of cleansing, and is a significant factor contributing to the detection of flat lesions: a randomized study. World J Gastroenterol. 2006;12:6161–6.
Fujii T, Hasegawa RT, Saitoh Y, Fleischer D, Saito Y, Sano Y, et al. Chromoscopy during colonoscopy. Endoscopy. 2001;33:1036–41.
Diamond GA. Reverend Bayes’ silent majority. An alternative factor affecting sensitivity and specificity of exercise electrocardiography. Am J Cardiol. 1986;57:1175–80.
Leiner S. Verification bias in screening for prostate cancer. N Engl J Med. 2003;349:1672–3.
Kosinski AS, Barnhart HX. A global sensitivity analysis of performance of a medical diagnostic test when verification bias is present. Stat Med. 2003;22:2711–21.
Murphy JR. The relationship of relative risk and positive predictive value in 2 × 2 tables. Am J Epidemiol. 1983;117:86–9.
Hewitson P, Glasziou P, Irwig L, Towler B, Watson E. Screening for colorectal cancer using the faecal occult blood test, hemoccult. Cochrane Database Syst Rev. 2007;1:CD001216.
Castiglione G, Sala P, Ciatto S, Grazzini G, Mazzotta A, Rossetti C, et al. Comparative analysis of results of guaiac and immunochemical tests for faecal occult blood in colorectal cancer screening in two oncological institutions. Eur J Cancer Prev. 1994;3:399–405.
Castiglione G, Zappa M, Grazzini G, Mazzotta A, Biagini M, Salvadori P, et al. Immunochemical vs guaiac faecal occult blood tests in a population-based screening programme for colorectal cancer. Br J Cancer. 1996;74:141–4.
Dancourt V, Lejeune C, Lepage C, Gailliard MC, Meny B, Faivre J. Immunochemical faecal occult blood tests are superior to guaiac-based tests for the detection of colorectal neoplasms. Eur J Cancer. 2008;44:2254–8.
Morikawa T, Kato J, Yamaji Y, Wada R, Mitsushima T, Shiratori Y. A comparison of the immunochemical fecal occult blood test and total colonoscopy in the asymptomatic population. Gastroenterology. 2005;129:422–8.
Zappa M, Castiglione G, Paci E, Grazzini G, Rubeca T, Turco P, et al. Measuring interval cancers in population-based screening using different assays of fecal occult blood testing: the District of Florence experience. Int J Cancer. 2001;92:151–4.
Smith A, Young GP, Cole SR, Bampton P. Comparison of a brush-sampling fecal immunochemical test for hemoglobin with a sensitive guaiac-based fecal occult blood test in detection of colorectal neoplasia. Cancer. 2006;107:2152–9.
Hol L, Van Leerdam ME, Van Ballegooijen M, Van Vuuren AJ, Van Dekken H, Reijerink JC, et al. Screening for colorectal cancer; randomised trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut. 2010;59:62–68.
Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–8.
Levi Z, Rozen P, Hazazi R, Vilkin A, Waked A, Maoz E, et al. A quantitative immunochemical fecal occult blood test for colorectal neoplasia. Ann Intern Med. 2007;146:244–55.
Subramanian S, Klosterman M, Amonkar MM, Hunt TL. Adherence with colorectal cancer screening guidelines: a review. Prev Med. 2004;38:536–50.
Gimeno-Garcia AZ, Quintero E, Nicolas-Perez D, Parra-Blanco A, Jimenez-Sosa A. Impact of an educational video-based strategy on the behavior process associated with colorectal cancer screening: a randomized controlled study. Cancer Epidemiol. 2009;33:216–22.
Irwig L, Bossuyt P, Glasziou P, Gatsonis C, Lijmer J. Designing studies to ensure that estimates of test accuracy are transferable. BMJ. 2002;324:669–71.
Acknowledgments
The authors wish to thank the participating patients, and the Staff of the Endoscopy Unit, University Hospital of the Canary Islands. They also thank Raquel Aguiar and Dr. Yasushi Sano for critical comments on the manuscript and Eiken Chemical Corp. for providing the OC-Light kits. This study was supported in part by grants from the Instituto de Salud Carlos III (C03/02), from the Consejería de Educación, Cultura y Deportes, Gobierno de Canarias (PI2002/138), and from the Fundación Canaria de Investigación (FUNCIS) (P21/02).
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Parra-Blanco and A. Z. Gimeno-García contributed equally to this work.
Rights and permissions
About this article
Cite this article
Parra-Blanco, A., Gimeno-García, A.Z., Quintero, E. et al. Diagnostic accuracy of immunochemical versus guaiac faecal occult blood tests for colorectal cancer screening. J Gastroenterol 45, 703–712 (2010). https://doi.org/10.1007/s00535-010-0214-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0214-8