Abstract
Background
A role of an altered dietary pattern (e.g., a diet rich in sugar) but also alterations at the level of the intestinal barrier have repeatedly been discussed to be involved in the development and progression of nonalcoholic fatty liver disease (NAFLD).
Aims
To determine if the nutritional intake, intestinal flora, and permeability and the development of NAFLD are related in humans.
Methods
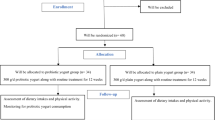
Ten controls and 20 patients with NAFLD ranging from simple steatosis to steatohepatitis were included in the study. Bacterial overgrowth, orocecal transit time, and intestinal permeability were assessed. Alcohol, endotoxin, and plasminogen activator inhibitor (PAI-) 1 concentration were determined in plasma. Nutritional intake was assessed using a dietary history.
Results
Despite no differences in the prevalence of bacterial overgrowth and in the orocecal transit time, intestinal permeability, alcohol, and endotoxin levels in plasma were significantly higher in patients with NAFLD than in controls. Similar results were also found for PAI-1 plasma concentrations. Patients with NAFLD had a significantly higher intake of protein, total carbohydrates, and mono- as well as disaccharides than controls. PAI-1, endotoxin, and ALT plasma levels were positively related to total protein and carbohydrate intake.
Conclusions
Taken together, our results indicate that intestinal permeability, endogenous alcohol synthesis, and nutritional intake are markedly altered in patients with NAFLD.


Similar content being viewed by others
Abbreviations
- ADH:
-
Alcohol dehydrogenase
- ALT:
-
Alanine-aminotransferase
- AST:
-
Aspartate-aminotransferase
- BMI:
-
Body mass index
- DBP:
-
Diastolic blood pressure
- γ-GT:
-
γ-Glutamyl transpeptidase
- HPAE-PAD:
-
High-performance-anion-exchange chromatography with pulsed amperometric detection
- LBP:
-
Lipopolysaccharide binding protein
- MUFA:
-
Monounsaturated fatty acids
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- OCTT:
-
Orocecal transit time
- PAI-1:
-
Plasminogen activator inhibitor 1
- PUFA:
-
Polyunsaturated fatty acids
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SEM:
-
Standard error of mean
- SFA:
-
Saturated fatty acids
- SIBO:
-
Small intestinal bacterial overgrowth
- TLR-4:
-
Toll-like receptor 4
- TNF-α:
-
Tumor necrosis factor alpha
References
Yang L, Bataller R, Dulyx J, et al. Attenuated hepatic inflammation and fibrosis in angiotensin type 1a receptor deficient mice. J Hepatol. 2005;43:317–323.
Adams LA, Lymp JF, St SJ, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121.
Bode C, Kugler V, Bode JC. Endotoxemia in patients with alcoholic and nonalcoholic cirrhosis and in subjects with no evidence of chronic liver disease following acute alcohol excess. J Hepatol. 1987;4:8–14.
Purohit V, Bode JC, Bode C, et al. Alcohol, intestinal bacterial growth, intestinal permeability to endotoxin, and medical consequences: summary of a symposium. Alcohol. 2008;42:349–361.
Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarhy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of nonalcoholic steatohepatitis. Gut. 2001;48:206–211.
Thuy S, Ladurner R, Volynets V, et al. Nonalcoholic fatty liver disease in humans is associated with increased plasma endotoxin and plasminogen activator inhibitor 1 concentrations and with fructose intake. J Nutr. 2008;138:1452–1455.
Soza A, Riquelme A, Gonzalez R, et al. Increased orocecal transit time in patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2005;50:1136–1140.
Harte AL, da Silva NF, Creely SJ, et al. Elevated endotoxin levels in nonalcoholic fatty liver disease. J Inflamm. 2010;7:15.
Farhadi A, Gundlapalli S, Shaikh M, et al. Susceptibility to gut leakiness: a possible mechanism for endotoxaemia in nonalcoholic steatohepatitis. Liver Int. 2008;28:1026–1033.
Ruiz AG, Casafont F, Crespo J, et al. Lipopolysaccharide-binding protein plasma levels and liver TNF-alpha gene expression in obese patients: evidence for the potential role of endotoxin in the pathogenesis of nonalcoholic steatohepatitis. Obes Surg. 2007;17:1374–1380.
Nair S, Cope K, Risby TH, Diehl AM. Obesity and female gender increase breath ethanol concentration: potential implications for the pathogenesis of nonalcoholic steatohepatitis. Am J Gastroenterol. 2001;96:1200–1204.
Assy N, Nasser G, Kamayse I, et al. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can J Gastroenterol. 2008;22:811–816.
Ouyang X, Cirillo P, Sautin Y, et al. Fructose consumption as a risk factor for nonalcoholic fatty liver disease. J Hepatol. 2008;48:993–999.
Solga S, Alkhuraishe AR, Clark JM, et al. Dietary composition and nonalcoholic fatty liver disease. Dig Dis Sci. 2004;49:1578–1583.
Abdelmalek MF, Suzuki A, Guy C, et al. Increased fructose consumption is associated with fibrosis severity in patients with nonalcoholic fatty liver disease. Hepatology. 2010;51:1961–1971.
Bergheim I, Weber S, Vos M, et al. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008;48:983–992.
Taylor KJ, Riely CA, Hammers L, et al. Quantitative US attenuation in normal liver and in patients with diffuse liver disease: importance of fat. Radiology. 1986;160:65–71.
Joseph AE, Dewbury KC, McGuire PG. Ultrasound in the detection of chronic liver disease (the “bright liver”). Br J Radiol. 1979;52:184–188.
Joseph AE, Saverymuttu SH, al-Sam S, Cook MG, Maxwell JD. Comparison of liver histology with ultrasonography in assessing diffuse parenchymal liver disease. Clin Radiol. 1991;43:26–31.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321.
Landig J, Erhardt JG, Bode JC, Bode C. Validation and comparison of two computerized methods of obtaining a diet history. Clin Nutr. 1998;17:113–117.
Erhardt JG, Meisner C, Bode JC, Bode C. Lycopene, beta-carotene, and colorectal adenomas 23. Am J Clin Nutr. 2003;78:1219–1224.
Generoso M, De RM, De RR, et al. Cellobiose and lactulose coupled with mannitol and determined using ion-exchange chromatography with pulsed amperometric detection, are reliable probes for investigation of intestinal permeability. J Chromatogr B Analyt Technol Biomed Life Sci. 2003;783:349–357.
Fleming SC, Kapembwa MS, Laker MF, Levin GE, Griffin GE. Rapid and simultaneous determination of lactulose and mannitol in urine, by HPLC with pulsed amperometric detection, for use in studies of intestinal permeability. Clin Chem. 1990;36:797–799.
Pascual S, Such J, Esteban A, et al. Intestinal permeability is increased in patients with advanced cirrhosis. Hepatogastroenterology. 2003;50:1482–1486.
Parrilli G, Cuomo R, Nardone G, Maio G, Izzo CM, Budillon G. Investigation of intestine function during acute viral hepatitis using combined sugar oral loads. Gut. 1987;28:1439–1444.
Liu H, Zhang S, Yu A, et al. Studies on intestinal permeability of cirrhotic patients by analysis lactulose and mannitol in urine with HPLC/RID/MS. Bioorg Med Chem Lett. 2004;14:2339–2344.
Cariello R, Federico A, Sapone A, et al. Intestinal permeability in patients with chronic liver diseases: Its relationship with the aetiology and the entity of liver damage. Dig Liver Dis. 2010;42:200–204.
Bonnichsen RK, Theorell H. An enzymatic method for the microdetermination of ethanol. Scand J Clin Lab Invest. 1951;3:58–62.
Parlesak A, Klein B, Schecher K, Bode JC. bode C. Prevalence of small bowel bacterial overgrowth and its association with nutrition intake in nonhospitalized older adults. J Am Geriatr Soc. 2003;51:768–773.
Miele L, Valenza V, La TG, et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology. 2009;49:1877–1887.
La Brooy SJ, Male PJ, Beavis AK, Misiewicz JJ. Assessment of the reproducibility of the lactulose H2 breath test as a measure of mouth to caecum transit time. Gut. 1983;24:893–896.
Toshimitsu K, Matsuura B, Ohkubo I, et al. Dietary habits and nutrient intake in nonalcoholic steatohepatitis. Nutrition. 2007;23:46–52.
Gill HK, Wu GY. Nonalcoholic fatty liver disease and the metabolic syndrome: effects of weight loss and a review of popular diets. Are low carbohydrate diets the answer? World J Gastroenterol. 2006;12:345–353.
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Long term nutritional intake and the risk for nonalcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47:711–717.
Kang H, Greenson JK, Omo JT, et al. Metabolic syndrome is associated with greater histologic severity, higher carbohydrate, and lower fat diet in patients with NAFLD. Am J Gastroenterol. 2006;101:2247–2253.
Yamamoto M, Iwasa M, Iwata K, et al. Restriction of dietary calories, fat and iron improves nonalcoholic fatty liver disease. J Gastroenterol Hepatol. 2007;22:498–503.
Ibrahim W, Lee US, Yeh CC, Szabo J, Bruckner G, Chow CK. Oxidative stress and antioxidant status in mouse liver: effects of dietary lipid, vitamin E and iron. 1656. J Nutr. 1997;127:1401–1406.
Cope K, Risby T, Diehl AM. Increased gastrointestinal ethanol production in obese mice: implications for fatty liver disease pathogenesis. Gastroenterology. 2000;119:1340–1347.
Logan BK, Jones AW. Endogenous ethanol production in a child with short gut syndrome. J Pediatr Gastroenterol Nutr. 2003;36:419–420.
McManus IR, Contag AO, Olson RE. Characterization of endogenous ethanol in the mammal. Science. 1960;131:102–103.
Baraona E, Julkunen R, Tannenbaum L, Lieber CS. Role of intestinal bacterial overgrowth in ethanol production and metabolism in rats. Gastroenterology. 1986;90:103–110.
Hanover LM, White JS. Manufacturing, composition, and applications of fructose. Am J Clin Nutr. 1993;58:724S–732S.
Mezey E, Imbembo AL, Potter JJ, Rent KC, Lombardo R, Holt RP. Endogenous ethanol production and hepatic disease following jejunoileal bypass for morbid obesity. Am J Clin Nutr. 1975;28:1277–1283.
Hunnisett A, Howard J, Davies S. Gut fermentation (or auto-brewery) syndrome. A new clinical test with initial observations and discussion of clinical and biological implications. J Nutr Med. 1990;1:33–38.
Rhodes JM, Middleton P, Jewell DP. The lactulose hydrogen breath test as a diagnostic test for small-bowel bacterial overgrowth. Scand J Gastroent. 1979;14:333–336.
Alessi MC, Bastelica D, Mavri A, et al. Plasma PAI-1 levels are more strongly related to liver steatosis than to adipose tissue accumulation. Arterioscler Thromb Vasc Biol. 2003;23:1262–1268.
Le KA, Bortolotti M. Role of dietary carbohydrates and macronutrients in the pathogenesis of nonalcoholic fatty liver disease. Curr Opin Clin Nutr Metab Care. 2008;11:477–482.
Acknowledgments
We would like to thank Prof. Dr. J.C. Bode and Prof. Dr. K.-P. Maier for their advice and the accompanying evaluation of the liver status of patients and controls included in the study. We further would like to thank Drs. C. Schäfer and K. Dirks for their assistance with the recruitment of patients for the study. We also would like to thank Prof. Dr. A. Heyar for his technical support with the determination of lactulose and mannitol concentrations in urine samples. This study was supported by a grant from the Center of Nutritional Medicine Hohenheim/Tübingen (PIs: AK and IB).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volynets, V., Küper, M.A., Strahl, S. et al. Nutrition, Intestinal Permeability, and Blood Ethanol Levels Are Altered in Patients with Nonalcoholic Fatty Liver Disease (NAFLD). Dig Dis Sci 57, 1932–1941 (2012). https://doi.org/10.1007/s10620-012-2112-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2112-9