Abstract
Background
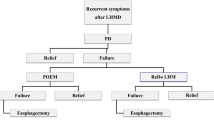
Achalasia is characterized by esophageal aperistalsis and impaired relaxation of the lower esophageal sphincter (LES). This contrasts with an insufficient LES, predisposing to gastro-esophageal reflux and Barrett’s esophagus. The co-incidence of achalasia and BE is rare. Pneumatic dilatation (PD) may lead to gastro-esophageal reflux, Barrett’s esophagus development, and esophageal adenocarcinoma.
Aims
To determine the incidence of Barrett’s esophagus and esophageal adenocarcinoma in achalasia patients treated with PD.
Methods
We performed a single-center cohort follow-up study of 331 achalasia patients treated with PD. Mean follow-up was 8.9 years, consisting of regular esophageal manometry, timed barium esophagram, and endoscopy.
Results
Twenty-eight (8.4 %) patients were diagnosed with Barrett’s esophagus, one at baseline endoscopy. This corresponds with an annual incidence of Barrett’s esophagus of 1.00 % (95 % CI 0.62–1.37). Hiatal herniation was present in 74 patients and 21 developed Barrett’s esophagus compared to seven of 257 patients without a hiatal hernia. Statistical analysis revealed a hazard ratio of 8.04 to develop Barrett’s esophagus if a hiatal hernia was present. Post-treatment LES pressures were lower in patients with Barrett’s esophagus than in those without (13.9 vs. 17.4 mmHg; p = 0.03). Two (0.6 %) patients developed esophageal adenocarcinoma during follow-up.
Conclusions
Barrett’s esophagus is incidentally diagnosed in untreated achalasia patients despite high LES pressures, but is more common after successful treatment, especially in the presence of hiatal herniation. Patients treated for achalasia should be considered for GERD treatment and surveillance of development of Barrett’s esophagus, in particular, when they have low LES pressures and a hiatal herniation.



Similar content being viewed by others
References
Mayberry JF. Epidemiology and demographics of achalasia. Gastrointest Endosc Clin North Am. 2001;11:235–248, v.
van Soest EM, Dieleman JP, Siersema PD, Sturkenboom MC, Kuipers EJ. Increasing incidence of Barrett’s oesophagus in the general population. Gut. 2005;54:1062–1066.
Cameron AJ, Lomboy CT. Barrett’s esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992;103:1241–1245.
Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831.
van Blankenstein M, Looman CW, Johnston BJ, Caygill CP. Age and sex distribution of the prevalence of Barrett’s esophagus found in a primary referral endoscopy center. Am J Gastroenterol. 2005;100:568–576.
de Jonge PJ, van Blankenstein M, Looman CW, Casparie MK, Meijer GA, Kuipers EJ. Risk of malignant progression in patients with Barrett’s oesophagus: a Dutch nationwide cohort study. Gut. 2010;59:1030–1036.
Kauer WK, Stein HJ. Role of acid and bile in the genesis of Barrett’s esophagus. Chest Surg Clin N Am. 2002;12:39–45.
Schoeman MN, Tippett MD, Akkermans LM, Dent J, Holloway RH. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology. 1995;108:83–91.
Walzer N, Hirano I. Achalasia. Gastroenterol Clin North Am. 2008;37:807–825, viii.
Alderliesten J, Conchillo JM, Leeuwenburgh I, Steyerberg EW, Kuipers EJ. Predictors for outcome of failure of balloon dilatation in patients with achalasia. Gut. 2011;60:10–16.
Reynolds JC, Parkman HP. Achalasia. Gastroenterol Clin North Am. 1989;18:223–255.
Leeuwenburgh I, Van Dekken H, Scholten P, et al. Oesophagitis is common in patients with achalasia after pneumatic dilatation. Aliment Pharmacol Ther. 2006;23:1197–1203.
Ellis FH Jr, Gibb SP, Balogh K, Schwaber JR. Esophageal achalasia and adenocarcinoma in Barrett’s esophagus: a report of two cases and a review of the literature. Dis Esophagus. 1997;10:55–60.
Guo JP, Gilman PB, Thomas RM, Fisher RS, Parkman HP. Barrett’s esophagus and achalasia. J Clin Gastroenterol. 2002;34:439–443.
Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henriquez A. Very late results of esophagomyotomy for patients with achalasia: clinical, endoscopic, histologic, manometric, and acid reflux studies in 67 patients for a mean follow-up of 190 months. Ann Surg. 2006;243:196–203.
Cantu P, Savojardo D, Baldoli D, Bonavina L, Penagini R. Barrett’s esophagus in untreated achalasia: ‘guess who’s coming to dinner’ first. Dis Esophagus. 2008;21:473.
Sikkema M, de Jonge PJ, Steyerberg EW, Kuipers EJ. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–244; quiz e232.
Shaheen NJ, Crosby MA, Bozymski EM, Sandler RS. Is there publication bias in the reporting of cancer risk in Barrett’s esophagus? Gastroenterology. 2000;119:333–338.
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816.
Burke CA, Achkar E, Falk GW. Effect of pneumatic dilation on gastroesophageal reflux in achalasia. Dig Dis Sci. 1997;42:998–1002.
Gerson LB, Shetler K, Triadafilopoulos G. Prevalence of Barrett’s esophagus in asymptomatic individuals. Gastroenterology. 2002;123:461–467.
Prach AT, MacDonald TA, Hopwood DA, Johnston DA. Increasing incidence of Barrett’s oesophagus: education, enthusiasm, or epidemiology? Lancet. 1997;350:933.
Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456.
Klinkenberg-Knol EC, Nelis F, Dent J, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661–669.
Spiess AE, Kahrilas PJ. Treating achalasia: from whalebone to laparoscope. JAMA. 1998;280:638–642.
Kuipers EJ. Barrett’s oesophagus, proton pump inhibitors and gastrin: the fog is clearing. Gut. 2010;59:148–149.
van Herwaarden MA, Samsom M, Smout AJ. Prolonged manometric recordings of oesophagus and lower oesophageal sphincter in achalasia patients. Gut. 2001;49:813–821.
Benini L, Sembenini C, Castellani G, et al. Pathological esophageal acidification and pneumatic dilitation in achalasic patients. Too much or not enough? Dig Dis Sci. 1996;41:365–371.
Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997;42:1354–1361.
Stamp DH. Three hypotheses linking bile to carcinogenesis in the gastrointestinal tract: certain bile salts have properties that may be used to complement chemotherapy. Med Hypotheses. 2002;59:398–405.
Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001;111:174S–177S.
Ott DJ, Gelfand DW, Chen YM, Wu WC, Munitz HA. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10:317–320.
Ott DJ, Hodge RG, Chen MY, Wu WC, Gelfand DW. Achalasia associated with hiatal hernia: prevalence and potential implications. Abdom Imaging. 1993;18:7–9.
Binder HJ, Clemett AR, Thayer WR, Spiro HM. Rarity of hiatus hernia in achalasia. N Engl J Med. 1965;272:680–682.
Olsen AM, Holman CB, Andersen HA. The diagnosis of cardiospasm. Dis Chest. 1953;23:477–498.
Taub W, Achkar E. Hiatal hernia in patients with achalasia. Am J Gastroenterol. 1987;82:1256–1258.
Goldenberg SP, Vos C, Burrell M, Traube M. Achalasia and hiatal hernia. Dig Dis Sci. 1992;37:528–531.
Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–616.
Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut Liver. 2011;5:267–277.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leeuwenburgh, I., Scholten, P., Caljé, T.J. et al. Barrett’s Esophagus and Esophageal Adenocarcinoma Are Common After Treatment for Achalasia. Dig Dis Sci 58, 244–252 (2013). https://doi.org/10.1007/s10620-012-2157-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2157-9