Abstract
Proton pump inhibitors (PPIs) are used to treat upper gastrointestinal tract disorders. Their efficacy and perceived safety have led to widespread prescription. This is not without effect, in terms of adverse events and resource utilization.
Aim
To prospectively assess oral PPI prescription in hospitalized patients.
Methods
PPI prescription in consecutive hospitalized patients was assessed. Indication and dose were assessed by patient interview and medical record review. Comparisons with current published prescribing guidelines were made.
Results
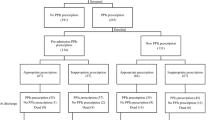
Four hundred and forty-seven patients were included. 57.5 % were prescribed PPIs. 26.8 % prescriptions were for inappropriate or unclear indications. 68.4 % were on higher doses than guidelines recommended, of which 41.6 % could have undergone dose reduction, and 26.5 % discontinued. In a multivariate analysis, age, gender, and length of stay had no association with PPI prescription. Although aspirin use was appropriately associated with PPI prescription (RR: 1.8, 95 % CI 1.127–3.69; p < 0.05), the PPI was often given at higher than recommended doses (p < 0.001). This may reflect older age and multiple risk factors in this subset. Surgical patients commenced more PPIs and at higher dosages (p < 0.001). Omeprazole and lansoprazole were most often inappropriately prescribed (p < 0.01, p < 0.001, respectively).
Conclusion
Inappropriate PPI therapy is still a problem in hospitals, though it appears to be at a lower level compared with previous studies. Awareness of evidence-based guidelines and targeted medicine reconciliation strategies are essential for cost-effective and safe use of these medications.



Similar content being viewed by others
Abbreviations
- PPI:
-
Proton pump inhibitor
- NSAID:
-
Nonsteroidal anti-inflammatories
- PUD:
-
Peptic ulcer disease
- GERD:
-
Gastro-esophageal reflux disease
- EGD:
-
Esophagogastroduodenoscopy
References
Wallander MA, Johansson S, Ruigómez A, Rodríguez LAG, Jones R. Dyspepsia in general practice: incidence, risk factors, comorbidity and mortality. Oxford J Med Family Pract. 2007;24:403–411.
Laheij RJ, Sturkenboom MC, Hassing RJ, et al. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA. 2004;292:1955–1960.
Aseeri M, Schroeder T, Kramer J, Zackula R. Gastric acid suppression by proton pump inhibitors as a risk factor for clostridium difficile-associated diarrhea in hospitalized patients. Am J Gastroenterol. 2008;103:2308–2313.
Gremmel T, Steiner S, Seidinger D, Koppensteiner R, Panzer S, Kopp CW. The influence of proton pump inhibitors on the antiplatelet potency of clopidogrel evaluated by 5 different platelet function tests. J Cardiovasc Pharmacol. 2010;56:532–539.
IMS Health Report. Leading therapy classes by global pharmaceutical sales. http://www.imshealth.com/ims/portal/front/articleC/0,2777,6025_80528184_80530441,00.html; 2006.
National Health Service. PACT centre pages. Drugs for dyspepsia. www.ppa.nhs.uk//news/pact-082004.htm; 2006.
van Vliet EP, Otten HJ, et al. Inappropriate prescription of proton pump inhibitors on two pulmonary medicine wards. Eur J Gastroenterol Hepatol. 2008;20:608–612.
Choudhry MN, Soran H, et al. Overuse and inappropriate prescribing of proton pump inhibitors in patients with Clostridium difficile-associated disease. QJM. 2008;101:445–448.
National Institute for Clinical Excellence. Dyspepsia: managing dyspepsia in adults in primary care. London: NICE; 2004.
BNF no. 66, September 2013–March 2014 ISBN-13: 978-0857110855.
McGowan B, Bennett K, Tilson L, Barry M. Cost effective prescribing of proton pump inhibitors (PPI’s) in the GMS Scheme. Ir Med J. 2005;98:78–80.
Molloy D, Molloy A, O’Loughlin C, Falconer M, Hennessy M. Inappropriate use of proton pump inhibitors. Ir J Med Sci. 2010;179:73–75. doi:10.1007/s11845-009-0426-1.
Thomas L, Culley EJ, Gladowski P, Goff V, Fong J, Marche SM. Longitudinal analysis of the costs associated with inpatient initiation and subsequent outpatient continuation of proton pump inhibitor therapy for stress ulcer prophylaxis in a large managed care organization. J Manag Care Pharm. 2010;16:122–129.
Targownik LE, Metge C, et al. The prevalence of and the clinical and demographic characteristics associated with high-intensity proton pump inhibitor use. Am J Gastroenterol. 2007;102:942–950.
Kaye K, Easton-Carter K, Brien J, Day R. An investigation of hospital prescribing of proton pump inhibitors[Internet]. Sydney: NSW Therapeutic Assessment Group. http://www.ciap.health.nsw.gov.au/nswtag/publications/reports/ppi_project_exec_summary_fv-0701.pdf; 2001.
Mat Saad AZ, Collins N, Lobo MM, O’Connor HJ. Proton pump inhibitors: a survey of prescribing in an Irish general hospital. Int J Clin Pract. 2005;59:31–34.
Forgacs I, Loganayagam A. Overprescribing proton pump inhibitors. BMJ. 2008;336:2.
Campbell F, Karnon J, Czoski-Murray C, Jones R. A systematic review of the effectiveness and cost-effectiveness of interventions aimed at preventing medication error (medicines reconciliation) at hospital admission. The University of Sheffield, School of Health and Related Research (ScHARR). J Eval Clin Pract. 2009;15:299–306.
Gerson LB, Robbins AS, Garber A, Hornberger J, Triadafilopoulos G. A cost-effectiveness analysis of prescribing strategies in the management of gastroeoesophageal reflux disease. Am J Gastroenterol. 2000;95:395–407.
Wilcox CM, Aillison J, Benzuly K, Borum M, Cryer B, Grosser T. Consensus development conference on the use of nonsteroidal anti-inflammatory agents, including cyclooxygenase-2 enzyme inhibitors and aspirin AGA Institute. Clin Gastro Hepatol. 2006;4:1082–1089.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelly, O.B., Dillane, C., Patchett, S.E. et al. The Inappropriate Prescription of Oral Proton Pump Inhibitors in the Hospital Setting: A Prospective Cross-Sectional Study. Dig Dis Sci 60, 2280–2286 (2015). https://doi.org/10.1007/s10620-015-3642-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3642-8