Abstract
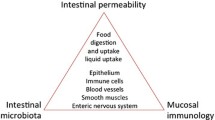
A major task of the intestine is to form a defensive barrier to prevent absorption of damaging substances from the external environment. This protective function of the intestinal mucosa is called permeability. Clinicians can use inert, nonmetabolized sugars such as mannitol, rhamnose, or lactulose to measure the permeability barrier or the degree of leakiness of the intestinal mucosa. Ample evidence indicates that permeability is increased in most patients with Crohn’s disease and in 10% to 20% of their clinically healthy relatives. The abnormal leakiness of the mucosa in Crohn’s patients and their relatives can be greatly amplified by aspirin preadministration. Permeability measurements in Crohn’s patients reflect the activity, extent, and distribution of the disease and may allow us predict the likelihood of recurrence after surgery or medically induced remission. Permeability is also increased in celiac disease and by trauma, burns, and nonsteroidal anti-inflammatory drugs. The major determinant of the rate of intestinal permeability is the opening or closure of the tight junctions between enterocytes in the paracellular space. As we broaden our understanding of the mechanisms and agents that control the degree of leakiness of the tight junctions, we will be increasingly able to use permeability measurements to study the etiology and pathogenesis of various disorders and to design or monitor therapies for their management.
Similar content being viewed by others
References and Recommended Reading
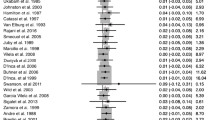
Bjarnason I, MacPherson A, Hollander D: Intestinal permeability: an overview. Gastroenterology 1995, 108:1566–1581. A very comprehensive review of the topic of permeability covering the period up to 1995. Includes an extensive bibliography and a good presentation of experimental and clinical information.
Hollander D: Intestinal permeability in health and disease. In Inflammatory Bowel Disease, edn 5. Edited by Kirsenr JB and Hanauer S. Philadelphia: WB Saunders; 1999; in press. The most up-to-date review of the clinical issues and applications of intestinal permeability.
Madara JL, Pappenheimer JR: Structural basis for physiological regulation of paracellular pathways in intestinal epithelia. J Membrane Biol 1987, 100:149–164.
Menzies, I.S: Transmucosal passage of inert molecules in health and disease. In In Intestinal Absorption and Secretion, Falk symposium 36. Edited by Skadhauge E, Heintze K. Baltimore: University Park Press; 1983:527–543.
Hollander D: The intestinal permeability barrier: a hypothesis as to its regulation and involvement in Crohn’s disease. Scand J Gastroenterol 1992, 27:721–726. This article details the experimental background supporting the hypothesis that clinical permeability measurements reflect the state of the paracellular tight junctions.
Pearson ADJ, Eastham EJ, Laker MF, et al.: Intestinal permeability in children with Crohn’s disease and celiac disease. Br Med J 1982, 285:20–21.
Ukabam SO, Clamp JR, Cooper BT: Abnormal small intestinal permeability to sugars in patients with Crohn’s disease of the terminal ileum and colon. Digestion 1983, 27:70–74.
Hollander D, Vadheim CM, Brettholz E, et al.: Increased intestinal permeability in Crohn’s patients and their relatives: an etiological factor. Ann Int Med 1986, 105:883–885. This is the seminal report demonstrating permeability abnormalities in clinically normal blood relatives of patients with Crohn’s disease.
Katz KD, Hollander D, Vadheim CM, et al.: Intestinal permeability in patients with Crohn’s disease and their healthy relatives. Gastroenterology 1989, 97:927–931.
May GR, Sutherland LR, Meddings JB: Is small intestinal permeability really increased in relatives of patients with Crohn’s disease? Gastroenterology 1993, 104:1627–1632.
Hollander D: Crohn’s disease: a permeability disorder of the tight-junction? Gut 1988, 29:621–1624.
Hollander D: Permeability in Crohn’s disease: altered barrier functions in healthy relatives? Gastroenterology 1993; 104:1848–1851.
Hollander D. The importance of intestinal permeability in the pathogenesis of Crohn’s disease. In Inflammatory Bowel Diseases, Falk Symposium 72. Edited by Rachmilewitz D. London: Kluwer Academic; 1994:41–51.
Pironi L, Miglioli M, Ruggeri E, et al.: Effect of non-steroidal anti-inflammatory drugs on intestinal permeability of first degree relatives of patients with Crohn’s disease [abstract]. Gastroenterology 1992, 102:A679.
Hilsden RJ, Meddings JB, Sutherland LR: Intestinal permeability changes in response to acetylsalicylic acid in relatives of patients with Crohn’s disease. Gastroenterology 1996, 110:1395–1403.
Peters M, Geypens B, Claus D, et al.: Clustering of increased small intestinal permeability in families with Crohn’s disease. Gastroenterology 1997,113:802–807.
Söderholm JD, Olaison G, Lindberg E, et al.: Different intestinal permeability patterns in relatives and spouses of patients with Crohn’s disease: an inherited defect in mucosal defence? Gut 1999, 44:96–100. This recent paper demonstrates that aspirin preadministration can greatly clarify the genetic basis of permeability abnormalities in the relatives of patients with Crohn’s disease.
Anderson JM, Van Itallie CM: Tight junctions and molecular basis for regulation of paracellular permeability. Am J Physiol 1995, 269:467–475.
Lee VHL, Yamamoto A, Kompella VB: Mucosal penetration enhancers for facilitation of peptide and protein drug absorption. Crit Rev Ther Drug Carrier Syst 1991, 8:91–192.
Hochman J, Artursson P: Mechanisms of absorption enhancement and tight junction regulation. J Controlled Release 1994, 29:253–267.
Fasano A, Baudry B, Pumplin DW, et al.: Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. Proc Natl Acad Sci U S A 1991, 88:5242–5246.
Fasano A, Fiorentini C, Donelli G, et al.: Zonula Occludens Toxin modulates tight junctions through protein kinase C-dependent actin reorganization, in vitro. J Clin Invest 1995, 96:710–720.
Fasano A, Uzzau S: Modulation of intestinal tight junctions by zonula occludens toxin permits enteral administration of insulin and other macromolecules in an animal model. J Clin Invest 1997, 99:158–164. An important demonstration of the therapeutic utility of manipulating the degree of permeability of the tight junctions.
Sanderson IR, Boulton P. Menzies IS, Walker-Smith JA: Improvement of abnormal lactulose/rhamnose permeability in active Crohn’s disease of the small bowel by an elemental diet. Gut 1987, 28:1073–1076.
Pironi L, Miglioli M, Ruggeri E, et al.: Relationship between intestinal permeability to 51Cr-EDTA and inflammatory activity in asymptomatic patients with Crohn’s disease. Dig Dis Sci 1990, 35:582–588.
Teahon K, Smethurst P, Pearson M, et al.: The effect of elemental diet on intestinal permeability and inflammation in Crohn’s disease. Gastroenterology 1991, 101:84–89.
Akram S, Morani S, Ou CN, et al.: Assessment of intestinal permeability with a two-hour urine collection. Dig Dis Sci 1998, 43:1946–1950.
Cox MA, Lewis KO, Cooper BT: Measurement of small intestinal permeability markers, lactulose, and mannitol in serum: results in celiac disease. Dig Dis Sci 1999, 44:402–406.
Wyatt J, Hubl W, Vogelsang H, Lochs H: Intestinal permeability predicts acute phases of Crohn’s disease [abstract]. Gastroenterology 1991, 100:A848.
Valpiani D, Ornigotti L, Ricca Rosellini S, et al.: Intestinal permeability: a non invasive method in predicting Crohn’s disease relapse [abstract]. Gastroenterology 1991, 100:A259.
Wyatt J, Vogelsang H, Hubl W, et al.: Intestinal permeability and the prediction of relapse in Crohn’s disease. Lancet 1993, 341:1437–1439.
Nejdfors P, Wang Q, Ekelund M, et al.: Increased colonic permeability in patients with ulcerative colitis: an in vitro study. Scand J Gastroenterol 1998, 33:749–753.
Miki K, Moore DJ, Butler RN, et al.: The sugar permeability test reflects disease activity in children and adolescents with inflammatory bowel disease. J Pediatr 1998, 133:750–754.
Pironi L, Miglioli M, Ruggeri E, et al.: Intestinal permeability (IP) to 51Cr-EDTA and postoperative recurrence of Crohn’s disease (CD): a follow-up study [abstract]. Gastroenterology 1991, 100:A239.
Krugliak P, Hollander D, Schlaepfer CC, et al.: Mechanisms and sites of mannitol permeability of small and large intestine in the rat. Dig Dis Sci 1994, 39:796–801.
Blomquist L, Oman H, Henriksson K, et al.: Increased absorption of polysucrose, a marker of intestinal paracellular permeability in Crohn’s disease. Eur J of Gastroenterol Hepatol 1993, 5:913–917.
Knight I: The development and applications of sucralose, a new high-intensity sweetener. Can J Physiol Pharmacol 1994, 72:435–439.
Meddings JB, Sutherland LR, Byles NI, Wallace JL: Sucrose: a novel permeability marker for gastroduodenal disease. Gastroenterology 1993, 104:1619–1626.
Jenkins AP, Nukajam WS, Menzies IS, Creamer B: Simultaneous administration of lactulose and 51Cr-ethylenediaminetetraacetic acid: a test to distinguish colonic from small-intestinal permeability change. Scand J Gastroenterol 1992, 27:769–773.
Bjarnason I, Peters TJ, Veall N: A persistent defect in intestinal permeability in celiac disease demonstrated by a [51Cr] labelled EDTA absorption test. Lancet 1983, 1(8336):1284–1285.
Ukabam SO, Cooper BT: Small intestinal permeability to mannitol, lactulose, and polyethylene glycol 400 in celiac disease. Dig Dis Sci 1984, 29:809–816.
Hamilton I, Cobden I, Axon ATR: Intestinal permeability in celiac disease: the response to gluten withdrawal and single dose gluten challenge. Gut 1982, 23:202–210.
Vogelsang H, Wyatt J, Penner E, et al.: Screening for celiac disease in first-degree relatives of patients with celiac disease by lactulose/mannitol test. Am J Gasteronenterol 1995, 90:1838–1842.
Bjarnason I, Peters TJ: Intestinal permeability, non-steroidal anti-inflammatory drug enteropathy and inflammatory bowel disease: an overview. Gut 1989, 30:22–28.
Bjarnason I, Haylar J. MacPherson AJ, Russell AS: Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology 1993, 104:1832–1847.
Marcial MA, Carlson SL, Madara JL: Partitioning of paracellular conductance along the ileal and crypt-villus axis: a hypothesis based on structural analysis with detailed consideration of tight junction structure-function relationship. J Membr Biol 1984, 80:59–70.
Harris CE, Griffiths RD, Freestone N, et al.: Intestinal permeability in the critically ill. Intensive Care Med 1992, 18:38–41.
Roumen RM, van der Vliet JA, et al.: Intestinal permeability is increased after major vascular surgery. J Vasc Surg 1993, 17:734–737.
Deitz EA: Intestinal permeability is increased in burn patients shortly after injury. Surgery 1990, 102:411–412.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hollander, D. Intestinal permeability, leaky gut, and intestinal disorders. Curr Gastroenterol Rep 1, 410–416 (1999). https://doi.org/10.1007/s11894-999-0023-5
Issue Date:
DOI: https://doi.org/10.1007/s11894-999-0023-5