Abstract
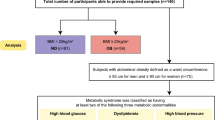
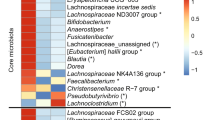
Emerging evidence has linked the gut microbiome to human obesity. We performed a metagenome-wide association study and serum metabolomics profiling in a cohort of lean and obese, young, Chinese individuals. We identified obesity-associated gut microbial species linked to changes in circulating metabolites. The abundance of Bacteroides thetaiotaomicron, a glutamate-fermenting commensal, was markedly decreased in obese individuals and was inversely correlated with serum glutamate concentration. Consistently, gavage with B. thetaiotaomicron reduced plasma glutamate concentration and alleviated diet-induced body-weight gain and adiposity in mice. Furthermore, weight-loss intervention by bariatric surgery partially reversed obesity-associated microbial and metabolic alterations in obese individuals, including the decreased abundance of B. thetaiotaomicron and the elevated serum glutamate concentration. Our findings identify previously unknown links between intestinal microbiota alterations, circulating amino acids and obesity, suggesting that it may be possible to intervene in obesity by targeting the gut microbiota.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Accession codes
References
Bäckhed, F. et al. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci. USA 101, 15718–15723 (2004).
Cox, A.J., West, N.P. & Cripps, A.W. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol. 3, 207–215 (2015).
Ridaura, V.K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Ley, R.E., Turnbaugh, P.J., Klein, S. & Gordon, J.I. Microbial ecology: human gut microbes associated with obesity. Nature 444, 1022–1023 (2006).
Turnbaugh, P.J. et al. A core gut microbiome in obese and lean twins. Nature 457, 480–484 (2009).
Karlsson, F.H. et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498, 99–103 (2013).
Qin, J. et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490, 55–60 (2012).
Le Chatelier, E. et al. Richness of human gut microbiome correlates with metabolic markers. Nature 500, 541–546 (2013).
Cotillard, A. et al. Dietary intervention impact on gut microbial gene richness. Nature 500, 585–588 (2013).
Furet, J.P. et al. Differential adaptation of human gut microbiota to bariatric surgery–induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 59, 3049–3057 (2010).
Kong, L.C. et al. Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am. J. Clin. Nutr. 98, 16–24 (2013).
Duncan, S.H. et al. Human colonic microbiota associated with diet, obesity and weight loss. Int. J. Obes. (Lond.) 32, 1720–1724 (2008).
Schwiertz, A. et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring) 18, 190–195 (2010).
Claesson, M.J. et al. Composition, variability and temporal stability of the intestinal microbiota of the elderly. Proc. Natl. Acad. Sci. USA 108 (Suppl. 1), 4586–4591 (2011).
Mueller, S. et al. Differences in fecal microbiota in different European study populations in relation to age, gender and country: a cross-sectional study. Appl. Environ. Microbiol. 72, 1027–1033 (2006).
David, L.A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014).
Li, J. et al. An integrated catalog of reference genes in the human gut microbiome. Nat. Biotechnol. 32, 834–841 (2014).
Everard, A. et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc. Natl. Acad. Sci. USA 110, 9066–9071 (2013).
Miquel, S. et al. Faecalibacterium prausnitzii and human intestinal health. Curr. Opin. Microbiol. 16, 255–261 (2013).
Peterson, C.T., Sharma, V., Elmén, L. & Peterson, S.N. Immune homeostasis, dysbiosis and therapeutic modulation of the gut microbiota. Clin. Exp. Immunol. 179, 363–377 (2015).
Yamauchi, T. et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat. Med. 7, 941–946 (2001).
Turnbaugh, P.J., Bäckhed, F., Fulton, L. & Gordon, J.I. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 3, 213–223 (2008).
Ulmer, J.E. et al. Characterization of glycosaminoglycan (GAG) sulfatases from the human gut symbiont Bacteroides thetaiotaomicron reveals the first GAG-specific bacterial endosulfatase. J. Biol. Chem. 289, 24289–24303 (2014).
Xu, J. et al. A genomic view of the human–Bacteroides thetaiotaomicron symbiosis. Science 299, 2074–2076 (2003).
Hooper, L.V. et al. Molecular analysis of commensal host–microbial relationships in the intestine. Science 291, 881–884 (2001).
Qian, C. & Cao, X. Regulation of Toll-like receptor signaling pathways in innate immune responses. Ann. NY Acad. Sci. 1283, 67–74 (2013).
Pedersen, H.K. et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 535, 376–381 (2016).
Shoaie, S. et al. Quantifying diet-induced metabolic changes of the human gut microbiome. Cell Metab. 22, 320–331 (2015).
Russell, W.R. et al. Major phenylpropanoid-derived metabolites in the human gut can arise from microbial fermentation of protein. Mol. Nutr. Food Res. 57, 523–535 (2013).
Wang, T.J. et al. Metabolite profiles and the risk of developing diabetes. Nat. Med. 17, 448–453 (2011).
Magnusson, M. et al. A diabetes-predictive amino acid score and future cardiovascular disease. Eur. Heart J. 34, 1982–1989 (2013).
Eckburg, P.B. et al. Diversity of the human intestinal microbial flora. Science 308, 1635–1638 (2005).
Bunyan, J., Murrell, E.A. & Shah, P.P. The induction of obesity in rodents by means of monosodium glutamate. Br. J. Nutr. 35, 25–39 (1976).
Dolnikoff, M., Martin-Hidalgo, A., Machado, U.F., Lima, F.B. & Herrera, E. Decreased lipolysis and enhanced glycerol and glucose utilization by adipose tissue prior to development of obesity in monosodium glutamate (MSG) treated-rats. Int. J. Obes. Relat. Metab. Disord. 25, 426–433 (2001).
Rubino, F. et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 39, 861–877 (2016).
Gralka, E. et al. Metabolomic fingerprint of severe obesity is dynamically affected by bariatric surgery in a procedure-dependent manner. Am. J. Clin. Nutr. 102, 1313–1322 (2015).
Lips, M.A. et al. Roux-en-Y gastric bypass surgery, but not calorie restriction, reduces plasma branched-chain amino acids in obese women independent of weight loss or the presence of type 2 diabetes. Diabetes Care 37, 3150–3156 (2014).
Mutch, D.M. et al. Metabolite profiling identifies candidate markers reflecting the clinical adaptations associated with Roux-en-Y gastric bypass surgery. PLoS One 4, e7905 (2009).
Gauffin Cano, P., Santacruz, A., Moya, Á. & Sanz, Y. Bacteroides uniformis CECT 7771 ameliorates metabolic and immunological dysfunction in mice with high-fat-diet induced obesity. PLoS One 7, e41079 (2012).
Mar Rodríguez, M. et al. Obesity changes the human gut mycobiome. Sci. Rep. 5, 14600 (2015).
Hermanussen, M. et al. Obesity, voracity and short stature: the impact of glutamate on the regulation of appetite. Eur. J. Clin. Nutr. 60, 25–31 (2006).
Olney, J.W. Brain lesions, obesity and other disturbances in mice treated with monosodium glutamate. Science 164, 719–721 (1969).
He, K. et al. Consumption of monosodium glutamate in relation to incidence of overweight in Chinese adults: China Health and Nutrition Survey (CHNS). Am. J. Clin. Nutr. 93, 1328–1336 (2011).
Comstock, L.E. & Coyne, M.J. Bacteroides thetaiotaomicron: a dynamic, niche-adapted human symbiont. BioEssays 25, 926–929 (2003).
Hooper, L.V., Falk, P.G. & Gordon, J.I. Analyzing the molecular foundations of commensalism in the mouse intestine. Curr. Opin. Microbiol. 3, 79–85 (2000).
Cuskin, F. et al. Human gut Bacteroidetes can utilize yeast mannan through a selfish mechanism. Nature 517, 165–169 (2015).
Vétizou, M. et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science 350, 1079–1084 (2015).
Wang, J. et al. Ablation of LGR4 promotes energy expenditure by driving white-to-brown fat switch. Nat. Cell Biol. 15, 1455–1463 (2013).
Liu, R. et al. Rare loss-of-function variants in NPC1 predispose to human obesity. Diabetes 66, 935–947 (2017).
Li, R. et al. SOAP2: an improved ultrafast tool for short read alignment. Bioinformatics 25, 1966–1967 (2009).
Feng, Q. et al. Gut microbiome development along the colorectal adenoma–carcinoma sequence. Nat. Commun. 6, 6528 (2015).
McArdle, B.H. & Anderson, M.J. Fitting multivariate models to community data: a comment on distance-based redundancy analysis. Ecology 82, 290–297 (2001).
Zapala, M.A. & Schork, N.J. Multivariate regression analysis of distance matrices for testing associations between gene expression patterns and related variables. Proc. Natl. Acad. Sci. USA 103, 19430–19435 (2006).
Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001).
Subramanian, S. et al. Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature 510, 417–421 (2014).
Luan, H. et al. Serum metabolomics reveals lipid metabolism variation between coronary artery disease and congestive heart failure: a pilot study. Biomarkers 18, 314–321 (2013).
Dunn, W.B. et al. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat. Protoc. 6, 1060–1083 (2011).
Wishart, D.S. et al. HMDB 3.0—The Human Metabolome Database in 2013. Nucleic Acids Res. 41, D801–D807 (2013).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30 (2000).
Zhang, C. et al. Dietary modulation of gut microbiota contributes to alleviation of both genetic and simple obesity in children. EBioMedicine 2, 968–984 (2015).
Zhang, X. et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat. Med. 21, 895–905 (2015).
Diggle, P.J., Heagerty, P., Liang, K.-Y. & Zeger, S.L. Analysis of Longitudinal Data 2nd edn (Oxford University Press, 2002).
Qian, S.W. et al. BMP4-mediated brown fat–like changes in white adipose tissue alter glucose and energy homeostasis. Proc. Natl. Acad. Sci. USA 110, E798–E807 (2013).
Wang, R.F., Cao, W.W. & Cerniglia, C.E. PCR detection and quantitation of predominant anaerobic bacteria in human and animal fecal samples. Appl. Environ. Microbiol. 62, 1242–1247 (1996).
Gao, X., Pujos-Guillot, E. & Sébédio, J.L. Development of a quantitative metabolomic approach to study clinical human fecal water metabolome based on trimethylsilylation derivatization and GC/MS analysis. Anal. Chem. 82, 6447–6456 (2010).
Tremaroli, V. et al. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab. 22, 228–238 (2015).
Acknowledgements
The authors thank the field workers for their contribution and the participants for their cooperation. We thank H.B. Nielsen, S.B. Pedersen and H. Zhao for their contribution to data discussions. We thank P. Yin, S. Wang and H. Yu for their assistance in cultivating bacteria. This study was supported by grants from National Natural Science Foundation of China (no. 81621061 (G.N.), 81522011 (J.W.), 81370963 (R.L.), 81570758 (R.L.), 81370949 (J.W.), 81570757 (J.W.), 81471060 (J.H.) and 81670761 (Y.G.)), National International Science Cooperation Foundation (no. 2015DFA30560, W.W.), 973 Foundation (no. 2015CB553600, G.N.) and Shenzhen Municipal Government of China (no. JSGG20140702161403250 (Q.F.), DRC-SZ[2015]162 (Q.F.), JSGG20160229172752028 (J.L.) and JCYJ20160229172757249 (H.J.)).
Author information
Authors and Affiliations
Contributions
W.W., K.K. and G.N. conceived and designed the project. W.W., G.N. J.H., R.L., Y.G. and Jiqiu Wang managed the study. J.H., J.S., Y.G., Y.Z., W.G., B.S., X.D., J.J. and Y.B. made clinical diagnosis, recruited subjects and performed intervention. J.S., P.L., L.X., X.Y., Wanyu Li, R.W., Y. Shen, M.Y. and Y. Sun collected samples and clinical phenotypes. Xiaoqiang Xu, Q.F., D.Z., Xiaokai Wang., H. Xia, Z. Lan, Z.J., J.L., H.Z., and H. Xie performed bioinformatics analyses. Z. Liu, F.L. and X.C. performed metabolomics profiling and data analysis. Xiaolin Wang., X.Z. and G.X. performed targeted amino acid profiling. S.Z. and Wen Liu conducted animal experiments. R.L., K.K., W.W., G.N. and Jiqiu Wang wrote the manuscript. L.M., L.Q., S.L., B.C., H.J., Xun Xu, H.Y. and Jian Wang contributed to text revision and discussion.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15 (PDF 5176 kb)
Supplementary Tables
Supplementary Tables 1–27 (XLSX 1519 kb)
Rights and permissions
About this article
Cite this article
Liu, R., Hong, J., Xu, X. et al. Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med 23, 859–868 (2017). https://doi.org/10.1038/nm.4358
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4358
This article is cited by
-
Gut microbiota profiling in obese children from Southeastern China
BMC Pediatrics (2024)
-
Integrative metagenomic analysis reveals distinct gut microbial signatures related to obesity
BMC Microbiology (2024)
-
ACOD1 deficiency offers protection in a mouse model of diet-induced obesity by maintaining a healthy gut microbiota
Cell Death & Disease (2024)
-
Resistant starch intake facilitates weight loss in humans by reshaping the gut microbiota
Nature Metabolism (2024)
-
Gamma-aminobutyric acid as a potential postbiotic mediator in the gut–brain axis
npj Science of Food (2024)