Key Points
-
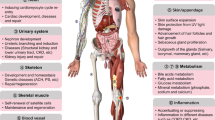
Fibroblast growth factors (FGFs) signal through FGF receptor tyrosine kinases to regulate a wide range of biological processes during development and adulthood.
-
FGF receptors (FGFRs) are involved in the pathogenesis of cancer and skeletal disorders. Experiments in model systems have shown that FGFR-specific inhibitors may be valuable in treating multiple myeloma, bladder and endometrial cancers.
-
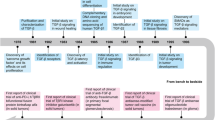
FGF1, FGF2 and FGF4 have been studied in clinical trials for the treatment of cardiovascular disease. The results of most of these trials have been unclear. However, some promising prospects remain. In particular, plasmids encoding FGF1 have shown potential in treating peripheral ischaemia.
-
Recombinant FGF7 is Food and Drug Administration approved for the treatment of chemoradiation-induced oral mucositis. Research into the application of FGF7 to treat conditions such as graft-versus-host disease is ongoing.
-
FGF18 increases cartilage formation in rats and may be useful in treating osteoarthritis.
-
The endocrine FGF19 subfamily holds the greatest promise for therapeutic development. These ligands circulate throughout the body owing to weak affinity for HSGAG (heparan sulphate glycosaminoglycan), and they require α-klotho–β-klotho proteins as cofactors for their activity. The α-klotho–β-klotho proteins also determine the target-tissue specificity of FGF19 subfamily ligands.
-
FGF19 negatively regulates bile acid synthesis and recombinant FGF19 increases the metabolic rate of mice. Unfortunately, FGF19 transgenic mice develop hepatocellular carcinomas, and this side effect may impede the pharmaceutical development of FGF19.
-
FGF21 is a mediator of the fasting response that increases glucose uptake, improves insulin sensitivity and reduces serum glucagon and triglyceride levels.
-
In contrast to FGF19, FGF21 is not mitogenic, and FGF21 administration leads to neither oedema nor hypoglycaemia, which are two common side effects of agents that modulate metabolic disorders. FGF21 thus shows great potential for treating type 2 diabetes.
-
FGF23 reduces renal phosphate reabsorption and downregulates vitamin D activation. FGF23 is broadly implicated in human disease, including autosomal-dominant hypophosphataemic rickets, tumour-induced osteomalacia, familial tumoral calcinosis and end-stage kidney disease. Neutralizing antibodies against FGF23 have shown efficacy in model systems and demonstrate the clinical potential of FGF23-specific therapies.
Abstract
The family of fibroblast growth factors (FGFs) regulates a plethora of developmental processes, including brain patterning, branching morphogenesis and limb development. Several mitogenic, cytoprotective and angiogenic therapeutic applications of FGFs are already being explored, and the recent discovery of the crucial roles of the endocrine-acting FGF19 subfamily in bile acid, glucose and phosphate homeostasis has sparked renewed interest in the pharmacological potential of this family. This Review discusses traditional applications of recombinant FGFs and small-molecule FGF receptor kinase inhibitors in the treatment of cancer and cardiovascular disease and their emerging potential in the treatment of metabolic syndrome and hypophosphataemic diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Itoh, N. & Ornitz, D. M. Evolution of the Fgf and Fgfr gene families. Trends Genet. 20, 563–569 (2004).
Olsen, S. K. et al. Fibroblast growth factor (FGF) homologous factors share structural but not functional homology with FGFs. J. Biol. Chem. 278, 34226–34236 (2003).
Fu, L. et al. Fibroblast growth factor19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology 145, 2594–2603 (2004).
Kharitonenkov, A. et al. FGF-21 as a novel metabolic regulator. J. Clin. Invest. 115, 1627–1635 (2005). The first paper to describe the metabolic profile of FGF21 in mice and rats.
Razzaque, M. S. & Lanske, B. The emerging role of the fibroblast growth factor-23-klotho axis in renal regulation of phosphate homeostasis. J. Endocrinol. 194, 1–10 (2007).
Tomlinson, E. et al. Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology 143, 1741–1747 (2002). Initiated interest in FGF19 as a metabolic regulator by detailing the phenotype of FGF19 transgenic mice.
White, K. E. et al. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nature Genet. 26, 345–348 (2000). This study showed that an FGF23 mutation caused ADHR, which began to unravel the physiology of FGF23.
Milunsky, J. M., Zhao, G., Maher, T. A., Colby, R. & Everman, D. B. LADD syndrome is caused by FGF10 mutations. Clin. Genet. 69, 349–354 (2006).
Tekin, M. et al. Homozygous mutations in fibroblast growth factor 3 are associated with a new form of syndromic deafness characterized by inner ear agenesis, microtia, and microdontia. Am. J. Hum. Genet. 80, 338–344 (2007).
Falardeau, J. et al. Decreased FGF8 signaling causes deficiency of gonadotropin-releasing hormone in humans and mice. J. Clin. Invest. 118, 2822–2831 (2008).
Revest, J. M., DeMoerlooze, L. & Dickson, C. Fibroblast growth factor 9 secretion is mediated by a non-cleaved amino-terminal signal sequence. J. Biol. Chem. 275, 8083–8090 (2000).
Nickel, W. Unconventional secretory routes: direct protein export across the plasma membrane of mammalian cells. Traffic 6, 607–614 (2005).
Mohammadi, M., Olsen, S. K. & Ibrahimi, O. A. Structural basis for fibroblast growth factor receptor activation. Cytokine Growth Factor Rev. 16, 107–137 (2005).
Goetz, R. et al. Molecular insights into the klotho-dependent, endocrine mode of action of fibroblast growth factor 19 subfamily members. Mol. Cell. Biol. 27, 3417–3428 (2007). Elucidates the structural rationale for the reduced binding of the FGF19 subfamily to heparan sulphate.
Wang, F., Kan, M., Yan, G., Xu, J. & McKeehan, W. L. Alternately spliced NH2-terminal immunoglobulin-like loop I in the ectodomain of the fibroblast growth factor (FGF) receptor 1 lowers affinity for both heparin and FGF-1. J. Biol. Chem. 270, 10231–10235 (1995).
Johnson, D. E., Lu, J., Chen, H., Werner, S. & Williams, L. T. The human fibroblast growth factor receptor genes: a common structural arrangement underlies the mechanisms for generating receptor forms that differ in their third immunoglobulin domain. Mol. Cell. Biol. 11, 4627–4634 (1991).
Ornitz, D. M. et al. Heparin is required for cell-free binding of basic fibroblast growth factor to a soluble receptor and for mitogenesis in whole cells. Mol. Cell. Biol. 12, 240–247 (1992).
Schlessinger, J. et al. Crystal structure of a ternary FGF–FGFR–heparin complex reveals a dual role for heparin in FGFR binding and dimerization. Mol. Cell 6, 743–750 (2000).
Yayon, A., Klagsbrun, M., Esko, J. D., Leder, P. & Ornitz, D. M. Cell surface, heparin-like molecules are required for binding of basic fibroblast growth factor to its high affinity receptor. Cell 64, 841–848 (1991).
Mohammadi, M. et al. Identification of six novel autophosphorylation sites on fibroblast growth factor receptor 1 and elucidation of their importance in receptor activation and signal transduction. Mol. Cell. Biol. 16, 977–989 (1996).
Dailey, L., Ambrosetti, D., Mansukhani, A. & Basilico, C. Mechanisms underlying differential responses to FGF signaling. Cytokine Growth Factor Rev. 16, 233–247 (2005).
Wiedlocha, A. & Sorensen, V. Signaling, internalization, and intracellular activity of fibroblast growth factor. Curr. Top. Microbiol. Immunol. 286, 45–79 (2004).
Orr-Urtreger, A. et al. Developmental localization of the splicing alternatives of fibroblast growth factor receptor-2 (FGFR2). Dev. Biol. 158, 475–486 (1993).
Grose, R. & Dickson, C. Fibroblast growth factor signaling in tumorigenesis. Cytokine Growth Factor Rev. 16, 179–186 (2005).
Ibrahimi, O. A. et al. Analysis of mutations in fibroblast growth factor (FGF) and a pathogenic mutation in FGF receptor (FGFR) provides direct evidence for the symmetric two-end model for FGFR dimerization. Mol. Cell. Biol. 25, 671–684 (2005).
Hacker, U., Nybakken, K. & Perrimon, N. Heparan sulphate proteoglycans: the sweet side of development. Nature Rev. Mol. Cell Biol. 6, 530–541 (2005).
Wu, D. Q., Kan, M. K., Sato, G. H., Okamoto, T. & Sato, J. D. Characterization and molecular cloning of a putative binding protein for heparin-binding growth factors. J. Biol. Chem. 266, 16778–16785 (1991).
Aigner, A. et al. An FGF-binding protein (FGF-BP) exerts its biological function by parallel paracrine stimulation of tumor cell and endothelial cell proliferation through FGF-2 release. Int. J. Cancer 92, 510–517 (2001).
Tassi, E. et al. Enhancement of fibroblast growth factor (FGF) activity by an FGF-binding protein. J. Biol. Chem. 276, 40247–40253 (2001).
Abuharbeid, S., Czubayko, F. & Aigner, A. The fibroblast growth factor-binding protein FGF-BP. Int. J. Biochem. Cell Biol. 38, 1463–1468 (2006).
Bottcher, R. T., Pollet, N., Delius, H. & Niehrs, C. The transmembrane protein XFLRT3 forms a complex with FGF receptors and promotes FGF signalling. Nature Cell Biol. 6, 38–44 (2004).
Hacohen, N., Kramer, S., Sutherland, D., Hiromi, Y. & Krasnow, M. A. sprouty encodes a novel antagonist of FGF signaling that patterns apical branching of the Drosophila airways. Cell 92, 253–263 (1998).
Cabrita, M. A. & Christofori, G. Sprouty proteins, masterminds of receptor tyrosine kinase signaling. Angiogenesis 11, 53–62 (2008).
Tsang, M. & Dawid, I. B. Promotion and attenuation of FGF signaling through the Ras-MAPK pathway. Sci. STKE 228, pe17 (2004).
Ibrahimi, O. A. et al. Structural basis for fibroblast growth factor receptor 2 activation in Apert syndrome. Proc. Natl Acad. Sci. USA 98, 7182–7187 (2001).
Dode, C. et al. Loss-of-function mutations in FGFR1 cause autosomal dominant Kallmann syndrome. Nature Genet. 33, 463–465 (2003).
Muenke, M. et al. A common mutation in the fibroblast growth factor receptor 1 gene in Pfeiffer syndrome. Nature Genet. 8, 269–274 (1994).
Rand, V. et al. Sequence survey of receptor tyrosine kinases reveals mutations in glioblastomas. Proc. Natl Acad. Sci. USA 102, 14344–14349 (2005).
Giri, D., Ropiquet, F. & Ittmann, M. Alterations in expression of basic fibroblast growth factor (FGF) 2 and its receptor FGFR-1 in human prostate cancer. Clin. Cancer Res. 5, 1063–1071 (1999).
Cross, N. C. & Reiter, A. Fibroblast growth factor receptor and platelet-derived growth factor receptor abnormalities in eosinophilic myeloproliferative disorders. Acta Haematol. 119, 199–206 (2008).
Kan, S. H. et al. Genomic screening of fibroblast growth-factor receptor 2 reveals a wide spectrum of mutations in patients with syndromic craniosynostosis. Am. J. Hum. Genet. 70, 472–486 (2002).
Chen, H. et al. A molecular brake in the kinase hinge region regulates the activity of receptor tyrosine kinases. Mol. Cell 27, 717–730 (2007).
Dutt, A. et al. Drug-sensitive FGFR2 mutations in endometrial carcinoma. Proc. Natl Acad. Sci. USA 105, 8713–8717 (2008).
Pollock, P. M. et al. Frequent activating FGFR2 mutations in endometrial carcinomas parallel germline mutations associated with craniosynostosis and skeletal dysplasia syndromes. Oncogene 26, 7158–7162 (2007).
Neilson, K. M. & Friesel, R. E. Constitutive activation of fibroblast growth factor receptor-2 by a point mutation associated with Crouzon syndrome. J. Biol. Chem. 270, 26037–26040 (1995).
Ibrahimi, O. A. et al. Biochemical analysis of pathogenic ligand-dependent FGFR2 mutations suggests distinct pathophysiological mechanisms for craniofacial and limb abnormalities. Hum. Mol. Genet. 13, 2313–2324 (2004).
Raybaud, C. & Di Rocco, C. Brain malformation in syndromic craniosynostoses, a primary disorder of white matter: a review. Childs Nerv. Syst. 23, 1379–1388 (2007).
Tanimoto, Y. et al. A soluble form of fibroblast growth factor receptor 2 (FGFR2) with S252W mutation acts as an efficient inhibitor for the enhanced osteoblastic differentiation caused by FGFR2 activation in Apert syndrome. J. Biol. Chem. 279, 45926–45934 (2004).
Antoniou, A. C. et al. Common breast cancer-predisposition alleles are associated with breast cancer risk in BRCA1 and BRCA2 mutation carriers. Am. J. Hum. Genet. 82, 937–948 (2008).
Webster, M. K. & Donoghue, D. J. FGFR activation in skeletal disorders: too much of a good thing. Trends Genet. 13, 178–182 (1997).
Naski, M. C., Wang, Q., Xu, J. & Ornitz, D. M. Graded activation of fibroblast growth factor receptor 3 by mutations causing achondroplasia and thanatophoric dysplasia. Nature Genet. 13, 233–237 (1996).
Passos-Bueno, M. R. et al. Clinical spectrum of fibroblast growth factor receptor mutations. Hum. Mutat. 14, 115–125 (1999).
Tavormina, P. L. et al. A novel skeletal dysplasia with developmental delay and acanthosis nigricans is caused by a Lys650Met mutation in the fibroblast growth factor receptor 3 gene. Am. J. Hum. Genet. 64, 722–731 (1999).
Rohmann, E. et al. Mutations in different components of FGF signaling in LADD syndrome. Nature Genet. 38, 414–417 (2006).
Chesi, M. et al. Frequent translocation t(4;14)(p16.3;q32.3) in multiple myeloma is associated with increased expression and activating mutations of fibroblast growth factor receptor 3. Nature Genet. 16, 260–264 (1997).
Cappellen, D. et al. Frequent activating mutations of FGFR3 in human bladder and cervix carcinomas. Nature Genet. 23, 18–20 (1999).
Hafner, C., Vogt, T. & Hartmann, A. FGFR3 mutations in benign skin tumors. Cell Cycle 5, 2723–2728 (2006).
Logie, A. et al. Activating mutations of the tyrosine kinase receptor FGFR3 are associated with benign skin tumors in mice and humans. Hum. Mol. Genet. 14, 1153–1160 (2005).
Wang, J., Stockton, D. W. & Ittmann, M. The fibroblast growth factor receptor-4 Arg388 allele is associated with prostate cancer initiation and progression. Clin. Cancer Res. 10, 6169–6178 (2004).
Streit, S. et al. Involvement of the FGFR4 Arg388 allele in head and neck squamous cell carcinoma. Int. J. Cancer 111, 213–217 (2004).
Meijer, D. et al. Fibroblast growth factor receptor 4 predicts failure on tamoxifen therapy in patients with recurrent breast cancer. Endocr. Relat. Cancer 15, 101–111 (2008).
Chow, L. Q. & Eckhardt, S. G. Sunitinib: from rational design to clinical efficacy. J. Clin. Oncol. 25, 884–896 (2007).
Grand, E. K., Chase, A. J., Heath, C., Rahemtulla, A. & Cross, N. C. Targeting FGFR3 in multiple myeloma: inhibition of t(4;14)-positive cells by SU5402 and PD173074. Leukemia 18, 962–966 (2004).
Meyer, A. N., McAndrew, C. W. & Donoghue, D. J. Nordihydroguaiaretic acid inhibits an activated fibroblast growth factor receptor 3 mutant and blocks downstream signaling in multiple myeloma cells. Cancer Res. 68, 7362–7370 (2008).
Byron, S. A. et al. Inhibition of activated fibroblast growth factor receptor 2 in endometrial cancer cells induces cell death despite PTEN abrogation. Cancer Res. 68, 6902–6907 (2008).
Martinez-Torrecuadrada, J. L. et al. Antitumor activity of fibroblast growth factor receptor 3-specific immunotoxins in a xenograft mouse model of bladder carcinoma is mediated by apoptosis. Mol. Cancer Ther. 7, 862–873 (2008).
Trudel, S. et al. The inhibitory anti-FGFR3 antibody, PRO-001, is cytotoxic to t(4;14) multiple myeloma cells. Blood 107, 4039–4046 (2006).
Roumiantsev, S. et al. Distinct stem cell myeloproliferative/T lymphoma syndromes induced by ZNF198–FGFR1 and BCR–FGFR1 fusion genes from 8p11 translocations. Cancer Cell 5, 287–298 (2004).
Miller, D. L., Ortega, S., Bashayan, O., Basch, R. & Basilico, C. Compensation by fibroblast growth factor 1 (FGF1) does not account for the mild phenotypic defects observed in FGF2 null mice. Mol. Cell. Biol. 20, 2260–2268 (2000).
Cuevas, P. et al. Hypotensive activity of fibroblast growth factor. Science 254, 1208–1210 (1991). One of the original papers on FGF1 physiology that helped lay the groundwork for the extensive study of FGF1 and FGF2 in clinical trials.
Cuevas, P. et al. Correction of hypertension by normalization of endothelial levels of fibroblast growth factor and nitric oxide synthase in spontaneously hypertensive rats. Proc. Natl Acad. Sci. USA 93, 11996–12001 (1996).
Zhou, M. et al. Fibroblast growth factor 2 control of vascular tone. Nature Med. 4, 201–207 (1998).
Dono, R., Texido, G., Dussel, R., Ehmke, H. & Zeller, R. Impaired cerebral cortex development and blood pressure regulation in FGF-2-deficient mice. EMBO J. 17, 4213–4225 (1998).
Ware, J. A. & Simons, M. Angiogenesis in ischemic heart disease. Nature Med. 3, 158–164 (1997).
Yanagisawa-Miwa, A. et al. Salvage of infarcted myocardium by angiogenic action of basic fibroblast growth factor. Science 257, 1401–1403 (1992).
Scholz, D., Cai, W. J. & Schaper, W. Arteriogenesis, a new concept of vascular adaptation in occlusive disease. Angiogenesis 4, 247–257 (2001).
Fulgham, D. L., Widhalm, S. R., Martin, S. & Coffin, J. D. FGF-2 dependent angiogenesis is a latent phenotype in basic fibroblast growth factor transgenic mice. Endothelium 6, 185–195 (1999).
Khurana, R. & Simons, M. Insights from angiogenesis trials using fibroblast growth factor for advanced arteriosclerotic disease. Trends Cardiovasc. Med. 13, 116–122 (2003).
Keller, M., Ruegg, A., Werner, S. & Beer, H. D. Active caspase-1 is a regulator of unconventional protein secretion. Cell 132, 818–831 (2008).
Bosse, Y. & Rola-Pleszczynski, M. FGF2 in asthmatic airway-smooth-muscle-cell hyperplasia. Trends Mol. Med. 14, 3–11 (2008).
Hutley, L. et al. Fibroblast growth factor 1: a key regulator of human adipogenesis. Diabetes 53, 3097–3106 (2004).
Iwakura, A. et al. Myocardial ischemia enhances the expression of acidic fibroblast growth factor in human pericardial fluid. Heart Vessels 15, 112–116 (2000).
Uriel, S., Brey, E. M. & Greisler, H. P. Sustained low levels of fibroblast growth factor-1 promote persistent microvascular network formation. Am. J. Surg. 192, 604–609 (2006).
Cuevas, P. et al. Fibroblast growth factor-1 prevents myocardial apoptosis triggered by ischemia reperfusion injury. Eur. J. Med. Res. 2, 465–468 (1997).
Schumacher, B., Pecher, P., von Specht, B. U. & Stegmann, T. Induction of neoangiogenesis in ischemic myocardium by human growth factors: first clinical results of a new treatment of coronary heart disease. Circulation 97, 645–650 (1998).
Comerota, A. J. et al. Naked plasmid DNA encoding fibroblast growth factor type 1 for the treatment of end-stage unreconstructible lower extremity ischemia: preliminary results of a phase I trial. J. Vasc. Surg. 35, 930–936 (2002).
Nikol, S. et al. Therapeutic angiogenesis with intramuscular NV1FGF improves amputation-free survival in patients with critical limb ischemia. Mol. Ther. 16, 972–978 (2008).
Ruck, A. & Sylven, C. Therapeutic angiogenesis gains a leg to stand on. Mol. Ther. 16, 808–810 (2008).
Cheng, H., Cao, Y. & Olson, L. Spinal cord repair in adult paraplegic rats: partial restoration of hind limb function. Science 273, 510–513 (1996).
Lin, P. H., Cheng, H., Huang, W. C. & Chuang, T. Y. Spinal cord implantation with acidic fibroblast growth factor as a treatment for root avulsion in obstetric brachial plexus palsy. J. Chin. Med. Assoc. 68, 392–396 (2005).
Lin, P. H., Chuang, T. Y., Liao, K. K., Cheng, H. & Shih, Y. S. Functional recovery of chronic complete idiopathic transverse myelitis after administration of neurotrophic factors. Spinal Cord 44, 254–257 (2006).
Cheng, H., Liao, K. K., Liao, S. F., Chuang, T. Y. & Shih, Y. H. Spinal cord repair with acidic fibroblast growth factor as a treatment for a patient with chronic paraplegia. Spine 29, E284–E288 (2004).
Unger, E. F. et al. Effects of a single intracoronary injection of basic fibroblast growth factor in stable angina pectoris. Am. J. Cardiol. 85, 1414–1419 (2000).
Laham, R. J. et al. Intracoronary and intravenous administration of basic fibroblast growth factor: myocardial and tissue distribution. Drug Metab. Dispos. 27, 821–826 (1999).
Simons, M. et al. Pharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: double-blind, randomized, controlled clinical trial. Circulation 105, 788–793 (2002).
Sellke, F. W., Laham, R. J., Edelman, E. R., Pearlman, J. D. & Simons, M. Therapeutic angiogenesis with basic fibroblast growth factor: technique and early results. Ann. Thorac. Surg. 65, 1540–1544 (1998).
Ruel, M. et al. Long-term effects of surgical angiogenic therapy with fibroblast growth factor 2 protein. J. Thorac. Cardiovasc. Surg. 124, 28–34 (2002).
Lazarous, D. F. et al. Basic fibroblast growth factor in patients with intermittent claudication: results of a phase I trial. J. Am. Coll. Cardiol. 36, 1239–1244 (2000).
Lederman, R. J. et al. Therapeutic angiogenesis with recombinant fibroblast growth factor-2 for intermittent claudication (the TRAFFIC study): a randomised trial. Lancet 359, 2053–2058 (2002).
D'Amato, R. J., Loughnan, M. S., Flynn, E. & Folkman, J. Thalidomide is an inhibitor of angiogenesis. Proc. Natl Acad. Sci. USA 91, 4082–4085 (1994).
Figg, W. D. et al. A randomized phase II trial of thalidomide, an angiogenesis inhibitor, in patients with androgen-independent prostate cancer. Clin. Cancer Res. 7, 1888–1893 (2001).
Eisen, T. et al. Continuous low dose Thalidomide: a phase II study in advanced melanoma, renal cell, ovarian and breast cancer. Br. J. Cancer 82, 812–817 (2000).
Myers, C. et al. Suramin: a novel growth factor antagonist with activity in hormone-refractory metastatic prostate cancer. J. Clin. Oncol. 10, 881–889 (1992).
Eisenberger, M. A. et al. Suramin, an active drug for prostate cancer: interim observations in a phase I trial. J. Natl Cancer Inst. 85, 611–621 (1993).
Motzer, R. J. et al. Phase II trial of suramin in patients with advanced renal cell carcinoma: treatment results, pharmacokinetics, and tumor growth factor expression. Cancer Res. 52, 5775–5779 (1992).
Walther, M. M., Figg, W. D. & Linehan, W. M. Intravesical suramin: a novel agent for the treatment of superficial transitional-cell carcinoma of the bladder. World J. Urol. 14, S8–S11 (1996).
Danesi, R. et al. Suramin inhibits bFGF-induced endothelial cell proliferation and angiogenesis in the chick chorioallantoic membrane. Br. J. Cancer 68, 932–938 (1993).
Zhang, Y., Song, S., Yang, F., Au, J. L. & Wientjes, M. G. Nontoxic doses of suramin enhance activity of doxorubicin in prostate tumors. J. Pharmacol. Exp. Ther. 299, 426–433 (2001).
Song, S., Wientjes, M. G., Gan, Y. & Au, J. L. Fibroblast growth factors: an epigenetic mechanism of broad spectrum resistance to anticancer drugs. Proc. Natl Acad. Sci. USA 97, 8658–8663 (2000).
Hawkins, M. J. Clinical trials of antiangiogenic agents. Curr. Opin. Oncol. 7, 90–93 (1995).
Sasisekharan, R., Shriver, Z., Venkataraman, G. & Narayanasami, U. Roles of heparan-sulphate glycosaminoglycans in cancer. Nature Rev. Cancer 2, 521–528 (2002).
Kudchadkar, R., Gonzalez, R. & Lewis, K. D. PI-88: a novel inhibitor of angiogenesis. Expert Opin. Investig. Drugs 17, 1769–1776 (2008).
Singh, R. K. et al. Interferons alpha and beta down-regulate the expression of basic fibroblast growth factor in human carcinomas. Proc. Natl Acad. Sci. USA 92, 4562–4566 (1995).
Dinney, C. P. et al. Inhibition of basic fibroblast growth factor expression, angiogenesis, and growth of human bladder carcinoma in mice by systemic interferon-α administration. Cancer Res. 58, 808–814 (1998).
Wang, Y. & Becker, D. Antisense targeting of basic fibroblast growth factor and fibroblast growth factor receptor-1 in human melanomas blocks intratumoral angiogenesis and tumor growth. Nature Med. 3, 887–893 (1997).
Presta, M. et al. Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev. 16, 159–178 (2005).
Kirkwood, J. M. et al. Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J. Clin. Oncol. 14, 7–17 (1996).
Hamm, C., Verma, S., Petrella, T., Bak, K. & Charette, M. Biochemotherapy for the treatment of metastatic malignant melanoma: a systematic review. Cancer Treat. Rev. 34, 145–156 (2008).
Rayburn, E. R. & Zhang, R. Antisense, RNAi, and gene silencing strategies for therapy: mission possible or impossible? Drug Discov. Today 13, 513–521 (2008).
Evans, S. J. et al. Dysregulation of the fibroblast growth factor system in major depression. Proc. Natl Acad. Sci. USA 101, 15506–15511 (2004).
Turner, C. A., Calvo, N., Frost, D. O., Akil, H. & Watson, S. J. The fibroblast growth factor system is downregulated following social defeat. Neurosci. Lett. 430, 147–150 (2008).
Turner, C. A., Gula, E. L., Taylor, L. P., Watson, S. J. & Akil, H. Antidepressant-like effects of intracerebroventricular FGF2 in rats. Brain Res. 1224, 63–68 (2008).
Ellman, M. B., An, H. S., Muddasani, P. & Im, H. J. Biological impact of the fibroblast growth factor family on articular cartilage and intervertebral disc homeostasis. Gene 420, 82–89 (2008).
Aviles, R. J., Annex, B. H. & Lederman, R. J. Testing clinical therapeutic angiogenesis using basic fibroblast growth factor (FGF-2). Br. J. Pharmacol. 140, 637–646 (2003).
Kitamura, M. et al. Periodontal tissue regeneration using fibroblast growth factor-2: randomized controlled phase II clinical trial. PLoS ONE 3, e2611 (2008).
Sugi, Y. et al. Fibroblast growth factor (FGF)-4 can induce proliferation of cardiac cushion mesenchymal cells during early valve leaflet formation. Dev. Biol. 258, 252–263 (2003).
Sun, X., Mariani, F. V. & Martin, G. R. Functions of FGF signalling from the apical ectodermal ridge in limb development. Nature 418, 501–508 (2002).
Feldman, B., Poueymirou, W., Papaioannou, V. E., DeChiara, T. M. & Goldfarb, M. Requirement of FGF-4 for postimplantation mouse development. Science 267, 246–249 (1995).
Hebert, J. M., Rosenquist, T., Gotz, J. & Martin, G. R. FGF5 as a regulator of the hair growth cycle: evidence from targeted and spontaneous mutations. Cell 78, 1017–1025 (1994).
Drogemuller, C., Rufenacht, S., Wichert, B. & Leeb, T. Mutations within the FGF5 gene are associated with hair length in cats. Anim. Genet. 38, 218–221 (2007).
Housley, D. J. & Venta, P. J. The long and the short of it: evidence that FGF5 is a major determinant of canine 'hair'-itability. Anim. Genet. 37, 309–315 (2006).
Armand, A. S., Laziz, I. & Chanoine, C. FGF6 in myogenesis. Biochim. Biophys. Acta 1763, 773–778 (2006).
Floss, T., Arnold, H. H. & Braun, T. A role for FGF-6 in skeletal muscle regeneration. Genes Dev. 11, 2040–2051 (1997).
Flynn, A. & O'Brien, T. Alferminogene tadenovec, an angiogenic FGF4 gene therapy for coronary artery disease. IDrugs 11, 283–293 (2008).
Grines, C. L. et al. Angiogenic Gene Therapy (AGENT) trial in patients with stable angina pectoris. Circulation 105, 1291–1297 (2002).
Henry, T. D. et al. Effects of Ad5FGF-4 in patients with angina: an analysis of pooled data from the AGENT-3 and AGENT-4 trials. J. Am. Coll. Cardiol. 50, 1038–1046 (2007).
Guo, L., Degenstein, L. & Fuchs, E. Keratinocyte growth factor is required for hair development but not for wound healing. Genes Dev. 10, 165–175 (1996).
Qiao, J. et al. FGF-7 modulates ureteric bud growth and nephron number in the developing kidney. Development 126, 547–554 (1999).
Werner, S. et al. Large induction of keratinocyte growth factor expression in the dermis during wound healing. Proc. Natl Acad. Sci. USA 89, 6896–6900 (1992).
Baskin, L. S. et al. Growth factors in bladder wound healing. J. Urol. 157, 2388–2395 (1997).
Ichimura, T., Finch, P. W., Zhang, G., Kan, M. & Stevens, J. L. Induction of FGF-7 after kidney damage: a possible paracrine mechanism for tubule repair. Am. J. Physiol. 271, F967–F976 (1996).
Kato, S. & Sekine, K. FGF–FGFR signaling in vertebrate organogenesis. Cell Mol. Biol. (Noisy-le-grand) 45, 631–638 (1999).
Umemori, H., Linhoff, M. W., Ornitz, D. M. & Sanes, J. R. FGF22 and its close relatives are presynaptic organizing molecules in the mammalian brain. Cell 118, 257–270 (2004).
Finch, P. W., Pricolo, V., Wu, A. & Finkelstein, S. D. Increased expression of keratinocyte growth factor messenger RNA associated with inflammatory bowel disease. Gastroenterology 110, 441–451 (1996).
Finch, P. W., Murphy, F., Cardinale, I. & Krueger, J. G. Altered expression of keratinocyte growth factor and its receptor in psoriasis. Am. J. Pathol. 151, 1619–1628 (1997).
Kovacs, D. et al. Immunohistochemical analysis of keratinocyte growth factor and fibroblast growth factor 10 expression in psoriasis. Exp. Dermatol. 14, 130–137 (2005).
Thomson, A. A. & Cunha, G. R. Prostatic growth and development are regulated by FGF10. Development 126, 3693–3701 (1999).
Yan, G., Fukabori, Y., Nikolaropoulos, S., Wang, F. & McKeehan, W. L. Heparin-binding keratinocyte growth factor is a candidate stromal-to-epithelial-cell andromedin. Mol. Endocrinol. 6, 2123–2128 (1992).
Spielberger, R. et al. Palifermin for oral mucositis after intensive therapy for hematologic cancers. N. Engl. J. Med. 351, 2590–2598 (2004). The results of this clinical trial helped bring FGF7 into use for the treatment of oral mucositis.
Potten, C. S. et al. Cell kinetic studies in the murine ventral tongue epithelium: the effects of repeated exposure to keratinocyte growth factor. Cell Prolif. 35 (Suppl. 1), 22–31 (2002).
Potten, C. S. et al. Cell kinetic studies in the murine ventral tongue epithelium: mucositis induced by radiation and its protection by pretreatment with keratinocyte growth factor (KGF). Cell Prolif. 35 (Suppl. 1), 32–47 (2002).
Braun, S. et al. Nrf2 transcription factor, a novel target of keratinocyte growth factor action which regulates gene expression and inflammation in the healing skin wound. Mol. Cell. Biol. 22, 5492–5505 (2002).
Ellison, C. A. et al. Effect of recombinant human keratinocyte growth factor (rHuKGF) on the immunopathogenesis of intestinal graft-vs-host disease induced without a preconditioning regimen. J. Clin. Immunol. 24, 197–211 (2004).
Panoskaltsis-Mortari, A. et al. Keratinocyte growth factor facilitates alloengraftment and ameliorates graft-versus-host disease in mice by a mechanism independent of repair of conditioning-induced tissue injury. Blood 96, 4350–4356 (2000).
Beaven, A. W. & Shea, T. C. The effect of palifermin on chemotherapy and radiation therapy-induced mucositis: a review of the current literature. Support Cancer Ther. 4, 188–197 (2007).
van der Velden, W. J., Herbers, A. H. & Blijlevens, N. M. Palifermin in allogeneic HSCT: many questions remain. Bone Marrow Transplant. 43, 85–86 (2008).
Werner, S. Keratinocyte growth factor: a unique player in epithelial repair processes. Cytokine Growth Factor Rev. 9, 153–165 (1998).
Freytes, C. O. et al. Phase I/II randomized trial evaluating the safety and clinical effects of repifermin administered to reduce mucositis in patients undergoing autologous hematopoietic stem cell transplantation. Clin. Cancer Res. 10, 8318–8324 (2004).
Sandborn, W. J. et al. Repifermin (keratinocyte growth factor-2) for the treatment of active ulcerative colitis: a randomized, double-blind, placebo-controlled, dose-escalation trial. Aliment. Pharmacol. Ther. 17, 1355–1364 (2003).
Liu, A. & Joyner, A. L. Early anterior/posterior patterning of the midbrain and cerebellum. Annu. Rev. Neurosci. 24, 869–896 (2001).
O'Leary, D. D., Chou, S. J. & Sahara, S. Area patterning of the mammalian cortex. Neuron 56, 252–269 (2007).
Meyers, E. N., Lewandoski, M. & Martin, G. R. An Fgf8 mutant allelic series generated by Cre- and Flp-mediated recombination. Nature Genet. 18, 136–141 (1998).
Xu, J., Liu, Z. & Ornitz, D. M. Temporal and spatial gradients of Fgf8 and Fgf17 regulate proliferation and differentiation of midline cerebellar structures. Development 127, 1833–1843 (2000).
Liu, Z., Xu, J., Colvin, J. S. & Ornitz, D. M. Coordination of chondrogenesis and osteogenesis by fibroblast growth factor 18. Genes Dev. 16, 859–869 (2002).
Ohbayashi, N. et al. FGF18 is required for normal cell proliferation and differentiation during osteogenesis and chondrogenesis. Genes Dev. 16, 870–879 (2002).
Ellsworth, J. L. et al. Fibroblast growth factor-18 is a trophic factor for mature chondrocytes and their progenitors. Osteoarthritis Cartilage 10, 308–320 (2002).
Moore, E. E. et al. Fibroblast growth factor-18 stimulates chondrogenesis and cartilage repair in a rat model of injury-induced osteoarthritis. Osteoarthritis Cartilage 13, 623–631 (2005).
Maruyama-Takahashi, K. et al. A neutralizing anti-fibroblast growth factor (FGF) 8 monoclonal antibody shows anti-tumor activity against FGF8b-expressing LNCaP xenografts in androgen-dependent and -independent conditions. Prostate 68, 640–650 (2008).
Shimada, N. et al. A neutralizing anti-fibroblast growth factor 8 monoclonal antibody shows potent antitumor activity against androgen-dependent mouse mammary tumors in vivo. Clin. Cancer Res. 11, 3897–3904 (2005).
Colvin, J. S., Green, R. P., Schmahl, J., Capel, B. & Ornitz, D. M. Male-to-female sex reversal in mice lacking fibroblast growth factor 9. Cell 104, 875–889 (2001).
Colvin, J. S., White, A. C., Pratt, S. J. & Ornitz, D. M. Lung hypoplasia and neonatal death in Fgf9-null mice identify this gene as an essential regulator of lung mesenchyme. Development 128, 2095–2106 (2001).
Lu, S. Y. et al. FGF-16 is required for embryonic heart development. Biochem. Biophys. Res. Commun. 373, 270–274 (2008).
van der Walt, J. M. et al. Fibroblast growth factor 20 polymorphisms and haplotypes strongly influence risk of Parkinson disease. Am. J. Hum. Genet. 74, 1121–1127 (2004).
Wang, G. et al. Variation in the miRNA-433 binding site of FGF20 confers risk for Parkinson disease by overexpression of α-synuclein. Am. J. Hum. Genet. 82, 283–289 (2008).
Ohmachi, S., Mikami, T., Konishi, M., Miyake, A. & Itoh, N. Preferential neurotrophic activity of fibroblast growth factor-20 for dopaminergic neurons through fibroblast growth factor receptor-1c. J. Neurosci. Res. 72, 436–443 (2003).
Takagi, Y. et al. Dopaminergic neurons generated from monkey embryonic stem cells function in a Parkinson primate model. J. Clin. Invest. 115, 102–109 (2005).
Schuster, M. W. et al. Safety and tolerability of velafermin (CG53135–05) in patients receiving high-dose chemotherapy and autologous peripheral blood stem cell transplant. Support Care Cancer 16, 477–483 (2008).
Kuro-o, M. et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390, 45–51 (1997). The first paper to describe the discovery of αklotho and its role in ageing in mice.
Kurosu, H. et al. Suppression of aging in mice by the hormone Klotho. Science 309, 1829–1833 (2005).
Imura, A. et al. Secreted Klotho protein in sera and CSF: implication for post-translational cleavage in release of Klotho protein from cell membrane. FEBS Lett. 565, 143–147 (2004).
Nabeshima, Y. The discovery of α-Klotho and FGF23 unveiled new insight into calcium and phosphate homeostasis. Cell. Mol. Life Sci. 65, 3218–3230 (2008).
Imura, A. et al. α-Klotho as a regulator of calcium homeostasis. Science 316, 1615–1618 (2007).
Chang, Q. et al. The β-glucuronidase klotho hydrolyzes and activates the TRPV5 channel. Science 310, 490–493 (2005).
Tsujikawa, H., Kurotaki, Y., Fujimori, T., Fukuda, K. & Nabeshima, Y. Klotho, a gene related to a syndrome resembling human premature aging, functions in a negative regulatory circuit of vitamin D endocrine system. Mol. Endocrinol. 17, 2393–2403 (2003).
Shimada, T. et al. Targeted ablation of Fgf23 demonstrates an essential physiological role of FGF23 in phosphate and vitamin D metabolism. J. Clin. Invest. 113, 561–568 (2004).
Kurosu, H. et al. Regulation of fibroblast growth factor-23 signaling by klotho. J. Biol. Chem. 281, 6120–6123 (2006). The first evidence that FGF23 requires α-klotho to activate FGFRs.
Urakawa, I. et al. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature 444, 770–774 (2006). References 186 and 187 showed, for the first time, that FGF23 requires α-klotho to activate FGFR1c.
Ito, S. et al. Impaired negative feedback suppression of bile acid synthesis in mice lacking βKlotho. J. Clin. Invest. 115, 2202–2208 (2005).
Inagaki, T. et al. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2, 217–225 (2005).
Yu, C. et al. Elevated cholesterol metabolism and bile acid synthesis in mice lacking membrane tyrosine kinase receptor FGFR4. J. Biol. Chem. 275, 15482–15489 (2000).
Kurosu, H. et al. Tissue-specific expression of βKlotho and fibroblast growth factor (FGF) receptor isoforms determines metabolic activity of FGF19 and FGF21. J. Biol. Chem. 282, 26687–26695 (2007).
Lin, B. C., Wang, M., Blackmore, C. & Desnoyers, L. R. Liver-specific activities of FGF19 require Klotho beta. J. Biol. Chem. 282, 27277–27284 (2007).
Wu, X. et al. Co-receptor requirements for fibroblast growth factor-19 signaling. J. Biol. Chem. 282, 29069–29072 (2007).
Kharitonenkov, A. et al. FGF-21/FGF-21 receptor interaction and activation is determined by βKlotho. J. Cell. Physiol. 215, 1–7 (2008).
Ogawa, Y. et al. βKlotho is required for metabolic activity of fibroblast growth factor 21. Proc. Natl Acad. Sci. USA 104, 7432–7437 (2007).
Suzuki, M. et al. βKlotho is required for fibroblast growth factor (FGF) 21 signaling through FGF receptor (FGFR) 1c and FGFR3c. Mol. Endocrinol. 22, 1006–1014 (2008).
Nishimura, T., Utsunomiya, Y., Hoshikawa, M., Ohuchi, H. & Itoh, N. Structure and expression of a novel human FGF, FGF-19, expressed in the fetal brain. Biochim. Biophys. Acta. 1444, 148–151 (1999).
Xie, M. H. et al. FGF-19, a novel fibroblast growth factor with unique specificity for FGFR4. Cytokine 11, 729–735 (1999).
Holt, J. A. et al. Definition of a novel growth factor-dependent signal cascade for the suppression of bile acid biosynthesis. Genes Dev. 17, 1581–1591 (2003).
Lundasen, T., Galman, C., Angelin, B. & Rudling, M. Circulating intestinal fibroblast growth factor 19 has a pronounced diurnal variation and modulates hepatic bile acid synthesis in man. J. Intern. Med. 260, 530–536 (2006). This interesting study revealed that FGF19 is induced following feeding in humans.
Choi, M. et al. Identification of a hormonal basis for gallbladder filling. Nature Med. 12, 1253–1255 (2006).
Harmer, N. J. et al. Towards a resolution of the stoichiometry of the fibroblast growth factor (FGF)–FGF receptor–heparin complex. J. Mol. Biol. 339, 821–834 (2004).
Dostalova, I. et al. Plasma concentrations of fibroblast growth factors 19 and 21 in patients with anorexia nervosa. J. Clin. Endocrinol. Metab. 93, 3627–3632 (2008).
Nicholes, K. et al. A mouse model of hepatocellular carcinoma: ectopic expression of fibroblast growth factor 19 in skeletal muscle of transgenic mice. Am. J. Pathol. 160, 2295–2307 (2002).
Desnoyers, L. R. et al. Targeting FGF19 inhibits tumor growth in colon cancer xenograft and FGF19 transgenic hepatocellular carcinoma models. Oncogene 27, 85–97 (2008).
Pai, R. et al. Inhibition of fibroblast growth factor 19 reduces tumor growth by modulating β-catenin signaling. Cancer Res. 68, 5086–5095 (2008).
Strack, A. M. & Myers, R. W. Modulation of metabolic syndrome by fibroblast growth factor 19 (FGF19)? Endocrinology 145, 2591–2593 (2004).
Nishimura, T., Nakatake, Y., Konishi, M. & Itoh, N. Identification of a novel FGF, FGF-21, preferentially expressed in the liver. Biochim. Biophys. Acta 1492, 203–206 (2000).
Zhang, X. et al. Serum FGF21 levels are increased in obesity and are independently associated with the metabolic syndrome in humans. Diabetes 57, 1246–1253 (2008).
Wente, W. et al. Fibroblast growth factor-21 improves pancreatic β-cell function and survival by activation of extracellular signal-regulated kinase 1/2 and Akt signaling pathways. Diabetes 55, 2470–2478 (2006).
Izumiya, Y. et al. FGF21 is an Akt-regulated myokine. FEBS Lett. 582, 3805–3810 (2008).
Coskun, T. et al. FGF21 corrects obesity in mice. Endocrinology 149, 6018–6027 (2008).
Xu, J. et al. FGF21 reverses hepatic steatosis, increases energy expenditure and improves insulin sensitivity in diet-induced obese mice. Diabetes 58, 250–259 (2009).
Inagaki, T. et al. Inhibition of growth hormone signaling by the fasting-induced hormone FGF21. Cell Metab. 8, 77–83 (2008).
Badman, M. K. et al. Hepatic fibroblast growth factor 21 is regulated by PPARα and is a key mediator of hepatic lipid metabolism in ketotic states. Cell Metab. 5, 426–437 (2007).
Kharitonenkov, A. et al. The metabolic state of diabetic monkeys is regulated by fibroblast growth factor-21. Endocrinology 148, 774–781 (2007).
Inagaki, T. et al. Endocrine regulation of the fasting response by PPARα-mediated induction of fibroblast growth factor 21. Cell Metab. 5, 415–425 (2007). References 215 and 217 describe the role of FGF21 in the fasting response.
Palou, M. et al. Sequential changes in the expression of genes involved in lipid metabolism in adipose tissue and liver in response to fasting. Pflugers Arch. 456, 825–836 (2008).
Reitman, M. L. FGF21: a missing link in the biology of fasting. Cell Metab. 5, 405–407 (2007).
Wang, H., Qiang, L. & Farmer, S. R. Identification of a domain within peroxisome proliferator-activated receptor γ regulating expression of a group of genes containing fibroblast growth factor 21 that are selectively repressed by SIRT1 in adipocytes. Mol. Cell. Biol. 28, 188–200 (2008).
Moyers, J. S. et al. Molecular determinants of FGF-21 activity-synergy and cross-talk with PPARγ signaling. J. Cell. Physiol. 210, 1–6 (2007).
Arner, P. et al. FGF21 attenuates lipolysis in human adipocytes — a possible link to improved insulin sensitivity. FEBS Lett. 582, 1725–1730 (2008).
Muise, E. S. et al. Adipose fibroblast growth factor 21 is up-regulated by peroxisome proliferator-activated receptor γ and altered metabolic states. Mol. Pharmacol. 74, 403–412 (2008).
Galman, C. et al. The circulating metabolic regulator FGF21 is induced by prolonged fasting and PPARα activation in man. Cell Metab. 8, 169–174 (2008).
Chen, W. W. et al. Circulating FGF-21 levels in normal subjects and in newly diagnose patients with type 2 diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 116, 65–68 (2008).
Yamashita, T., Yoshioka, M. & Itoh, N. Identification of a novel fibroblast growth factor, FGF-23, preferentially expressed in the ventrolateral thalamic nucleus of the brain. Biochem. Biophys. Res. Commun. 277, 494–498 (2000).
Riminucci, M. et al. FGF-23 in fibrous dysplasia of bone and its relationship to renal phosphate wasting. J. Clin. Invest. 112, 683–692 (2003).
Liu, S. et al. Regulation of fibroblastic growth factor 23 expression but not degradation by PHEX. J. Biol. Chem. 278, 37419–37426 (2003).
Bai, X. Y., Miao, D., Goltzman, D. & Karaplis, A. C. The autosomal dominant hypophosphatemic rickets R176Q mutation in fibroblast growth factor 23 resists proteolytic cleavage and enhances in vivo biological potency. J. Biol. Chem. 278, 9843–9849 (2003).
Larsson, T. et al. Transgenic mice expressing fibroblast growth factor 23 under the control of the α1(I) collagen promoter exhibit growth retardation, osteomalacia, and disturbed phosphate homeostasis. Endocrinology 145, 3087–3094 (2004).
Fukumoto, S. Physiological regulation and disorders of phosphate metabolism — pivotal role of fibroblast growth factor 23. Intern. Med. 47, 337–343 (2008).
Saito, H. et al. Human fibroblast growth factor-23 mutants suppress Na+-dependent phosphate co-transport activity and 1α, 25-dihydroxyvitamin D3 production. J. Biol. Chem. 278, 2206–2211 (2003).
Segawa, H. et al. Effect of hydrolysis-resistant FGF23–R179Q on dietary phosphate regulation of the renal type-II Na/Pi transporter. Pflugers Arch. 446, 585–592 (2003).
Ben-Dov, I. Z. et al. The parathyroid is a target organ for FGF23 in rats. J. Clin. Invest. 117, 4003–4008 (2007).
Sitara, D. et al. Homozygous ablation of fibroblast growth factor-23 results in hyperphosphatemia and impaired skeletogenesis, and reverses hypophosphatemia in Phex-deficient mice. Matrix Biol. 23, 421–432 (2004).
Hesse, M., Frohlich, L. F., Zeitz, U., Lanske, B. & Erben, R. G. Ablation of vitamin D signaling rescues bone, mineral, and glucose homeostasis in Fgf-23 deficient mice. Matrix Biol. 26, 75–84 (2007).
Razzaque, M. S., Sitara, D., Taguchi, T., St-Arnaud, R. & Lanske, B. Premature aging-like phenotype in fibroblast growth factor 23 null mice is a vitamin D-mediated process. FASEB J. 20, 720–722 (2006).
Sitara, D. et al. Genetic ablation of vitamin D activation pathway reverses biochemical and skeletal anomalies in Fgf-23-null animals. Am. J. Pathol. 169, 2161–2170 (2006).
Kuro-o, M. Klotho as a regulator of fibroblast growth factor signaling and phosphate/calcium metabolism. Curr. Opin. Nephrol. Hypertens. 15, 437–441 (2006).
Inoue, Y. et al. Role of the vitamin D receptor in FGF23 action on phosphate metabolism. Biochem. J. 390, 325–331 (2005).
Medici, D. et al. FGF-23-Klotho signaling stimulates proliferation and prevents vitamin D-induced apoptosis. J. Cell Biol. 182, 459–465 (2008).
A gene (PEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. The HYP Consortium. Nature Genet. 11, 130–136 (1995).
Jonsson, K. B. et al. Fibroblast growth factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N. Engl. J. Med. 348, 1656–1663 (2003).
Yamazaki, Y. et al. Increased circulatory level of biologically active full-length FGF-23 in patients with hypophosphatemic rickets/osteomalacia. J. Clin. Endocrinol. Metab. 87, 4957–4960 (2002).
Weber, T. J., Liu, S., Indridason, O. S. & Quarles, L. D. Serum FGF23 levels in normal and disordered phosphorus homeostasis. J. Bone Miner. Res. 18, 1227–1234 (2003).
Shulman, D. I. et al. Tumor-induced rickets: usefulness of MR gradient echo recall imaging for tumor localization. J. Pediatr. 144, 381–385 (2004).
Lyles, K. W. et al. Genetic transmission of tumoral calcinosis: autosomal dominant with variable clinical expressivity. J. Clin. Endocrinol. Metab. 60, 1093–1096 (1985).
Araya, K. et al. A novel mutation in fibroblast growth factor 23 gene as a cause of tumoral calcinosis. J. Clin. Endocrinol. Metab. 90, 5523–5527 (2005).
Benet-Pages, A., Orlik, P., Strom, T. M. & Lorenz-Depiereux, B. An FGF23 missense mutation causes familial tumoral calcinosis with hyperphosphatemia. Hum. Mol. Genet. 14, 385–390 (2005).
Larsson, T. et al. A novel recessive mutation in fibroblast growth factor-23 causes familial tumoral calcinosis. J. Clin. Endocrinol. Metab. 90, 2424–2427 (2005).
Ichikawa, S. et al. A homozygous missense mutation in human KLOTHO causes severe tumoral calcinosis. J. Musculoskelet. Neuronal Interact. 7, 318–319 (2007).
Shimada, T. et al. Mutant FGF-23 responsible for autosomal dominant hypophosphatemic rickets is resistant to proteolytic cleavage and causes hypophosphatemia in vivo. Endocrinology 143, 3179–3182 (2002).
Kato, K. et al. Polypeptide GalNAc-transferase T3 and familial tumoral calcinosis. Secretion of fibroblast growth factor 23 requires O-glycosylation. J. Biol. Chem. 281, 18370–18377 (2006).
Topaz, O. et al. Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nature Genet. 36, 579–581 (2004).
Imanishi, Y. et al. FGF-23 in patients with end-stage renal disease on hemodialysis. Kidney Int. 65, 1943–1946 (2004).
Larsson, T., Nisbeth, U., Ljunggren, O., Juppner, H. & Jonsson, K. B. Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int. 64, 2272–2279 (2003).
Razzaque, M. S. Does FGF23 toxicity influence the outcome of chronic kidney disease? Nephrol. Dial. Transplant. 24, 4–7 (2009).
Gutierrez, O. M. et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N. Engl. J. Med. 359, 584–592 (2008). This study shows a correlation between serum FGF23 levels and chronic kidney disease mortality. This area requires further research, as the role of FGF23 in chronic kidney disease is poorly understood.
Nakanishi, S. et al. Serum fibroblast growth factor-23 levels predict the future refractory hyperparathyroidism in dialysis patients. Kidney Int. 67, 1171–1178 (2005).
Aono Y, et al. The neutralization of FGF-23 ameliorates hypophosphatemia and rickets in Hyp mice. J. Bone Miner. Res. 18, S16 (2003).
Yamazaki, Y. et al. Anti-FGF23 neutralizing antibodies demonstrate the physiological role and structural features of FGF23. J. Bone Miner. Res. 23, 1509–1518 (2008).
Turner, C. A., Akil, H., Watson, S. J. & Evans, S. J. The fibroblast growth factor system and mood disorders. Biol. Psychiatry 59, 1128–1135 (2006).
Goldfarb, M. Fibroblast growth factor homologous factors: evolution, structure, and function. Cytokine Growth Factor Rev. 16, 215–220 (2005).
Dor, Y. et al. Conditional switching of VEGF provides new insights into adult neovascularization and pro-angiogenic therapy. EMBO J. 21, 1939–1947 (2002).
Bush, M. A. et al. Pharmacokinetics and pharmacodynamics of recombinant FGF-2 in a phase I trial in coronary artery disease. J. Clin. Pharmacol. 41, 378–385 (2001).
Nugent, M. A. & Edelman, E. R. Kinetics of basic fibroblast growth factor binding to its receptor and heparan sulfate proteoglycan: a mechanism for cooperactivity. Biochemistry 31, 8876–8883 (1992).
Ortega, S. et al. Conversion of cysteine to serine residues alters the activity, stability, and heparin dependence of acidic fibroblast growth factor. J. Biol. Chem. 266, 5842–5846 (1991).
Dubey, V. K., Lee, J., Somasundaram, T., Blaber, S. & Blaber, M. Spackling the crack: stabilizing human fibroblast growth factor-1 by targeting the N and C terminus β-strand interactions. J. Mol. Biol. 371, 256–268 (2007).
Rajanayagam, M. A. et al. Intracoronary basic fibroblast growth factor enhances myocardial collateral perfusion in dogs. J. Am. Coll. Cardiol. 35, 519–526 (2000).
Lazarous, D. F. et al. Pharmacodynamics of basic fibroblast growth factor: route of administration determines myocardial and systemic distribution. Cardiovasc. Res. 36, 78–85 (1997).
Post, M. J., Laham, R., Sellke, F. W. & Simons, M. Therapeutic angiogenesis in cardiology using protein formulations. Cardiovasc. Res. 49, 522–531 (2001).
Yla-Herttuala, S. & Martin, J. F. Cardiovascular gene therapy. Lancet 355, 213–222 (2000).
Kornowski, R., Fuchs, S., Leon, M. B. & Epstein, S. E. Delivery strategies to achieve therapeutic myocardial angiogenesis. Circulation 101, 454–458 (2000).
Lee, R. J. et al. VEGF gene delivery to myocardium: deleterious effects of unregulated expression. Circulation 102, 898–901 (2000).
Celletti, F. L. et al. Vascular endothelial growth factor enhances atherosclerotic plaque progression. Nature Med. 7, 425–429 (2001).
Simons, M. et al. Clinical trials in coronary angiogenesis: issues, problems, consensus: an expert panel summary. Circulation 102, E73–E86 (2000).
Presta, M. et al. Heparin derivatives as angiogenesis inhibitors. Curr. Pharm. Des. 9, 553–566 (2003).
Goetz, R. et al. Crystal structure of a fibroblast growth factor homologous factor defines conserved surface for binding and modulation of voltage-gated sodium channels. J. Biol. Chem. (in the press).
Acknowledgements
This work was supported by the US National Institutes of Health (NIH) grant R01-DE13686 (to M.M.) and by NIH/NIGMS training grant T32-GM066704-05 (to A.B.).
Author information
Authors and Affiliations
Related links
Glossary
- Autosomal dominant hypophosphataemic rickets
-
A hereditary disorder of phosphate wasting characterized by rickets, lower extremity deformities and osteomalacia.
- Lacrimo-auriculo-dento-digital syndrome
-
(LADD). A syndrome characterized by abnormalities of the digits and teeth, low-set ears and aplasia of the lacrimal and salivary glands. Mutations in FGFR2 and FGF10 are known to cause LADD.
- Kallmann syndrome
-
This syndrome results from a deficiency of gonadotropin-releasing hormone, which leads to hypogonadism. Mutations in FGFR1c and FGF8 are known to cause Kallmann syndrome.
- Oral mucositis
-
This condition results from injury to the epithelium of the oral cavity and can vary widely in severity. In the worst cases, oral mucositis can lead to ulceration, infection and the need for assisted feeding.
- Heparan sulphate glycosaminoglycan
-
(HSGAG). HSGAGs are long chains of repeating disaccharide units that can be variably sulphated or acetylated, allowing for considerable structural diversity. HSGAGs are located in the extracellular matrix at the surface of every cell, where they modulate the activity of a wide range of growth factors and morphogens.
- Exon skipping
-
A specific type of alternative splicing in which an exon is entirely skipped.
- Alternative splicing
-
This process increases protein diversity by dividing up the primary RNA gene transcript, excluding certain exons, and then reconnecting the transcript. These alternative ribonucleotide sequences are then translated, giving a variety of protein isoforms.
- Craniosynostosis
-
This condition results from the premature closure of sutures of a developing skull before the completion of brain growth. The brain continues to grow in areas of the skull where sutures have not closed, leading to a malformed cranium.
- Apert's syndrome
-
One of the most common craniosynostosis syndromes that exhibits severe syndactyly (digit fusion) of the hands and feet. Apert's syndrome is often associated with visceral abnormalities of the cardiovascular, respiratory and urogenital systems.
- Osteoglophonic dysplasia
-
A bone disorder presenting with dwarfism, vertebral fragility, craniosynostosis and failure to thrive. The term osteoglophonic refers to the 'hollowed out' appearance of the metaphyses in X-rays, which are the growth zones of long bones.
- Pfeiffer's syndrome
-
A craniosynostosis disorder that can also present with polydactyly.
- Glioblastoma
-
An aggressive tumour derived from glial cells that exhibits high levels of neovascularization.
- Myeloproliferative syndrome
-
A progressive disease that can transform into acute leukaemia. Also known as stem cell leukaemia or lymphoma syndrome, it often presents with a T-cell lymphoblastic lymphoma and eosinophilia.
- Crouzon's syndrome
-
A craniosynostosis syndrome presenting with a beaked nose and bulging, excessively separated eyes (exopthalmos and hypertelorism, respectively).
- Callosal agenesis
-
An absence of the corpus callosum, the tissue that connects the two hemispheres of the brain.
- Ventriculomegaly
-
A condition associated with enlarged lateral ventricles in the brain. Ventriculomegaly can have many causes, one of which is callosal agenesis.
- Hypochrondroplasia
-
A mild dwarfism syndrome generally presenting with nearly normal cranial and facial characteristics.
- Thanatophoric dysplasia type II
-
A lethal neonatal skeletal dysplasia associated with a severe cloverleaf-shaped skull deformity.
- Severe achondroplasia with developmental delay and acanthosis nigricans syndrome
-
This dwarfism syndrome is accompanied by substantial neurological disorders and acanthosis nigricans, which involves a hyperpigmentation of the skin.
- Nitric oxide
-
Among its many functions, this small molecule relaxes the smooth muscle surrounding blood vessels.
- Brachial plexus
-
The bundle of nerves located in the axilla (armpit) that descends into the upper limb to provide sensation and motor control.
- Chronic transverse myelitis
-
Inflammation across the width of one segment of the spinal cord that can lead to destruction of myelin and neurological impairment.
- Heparin
-
A highly sulphated heparan sulphate glycosaminoglycan (HSGAG). Although it does not act physiologically on FGF–FGFR signalling, it can substitute for other HSGAGs in experimental studies.
- Trophoblast
-
These cells form the outer layer of the developing embryo and are responsible for its implantation into the endometrium.
- Osteomalacia
-
Demineralization of the bones often associated with a lack of vitamin D.
- Secondary hyperparathyroidism
-
This condition is marked by excessive secretion of parathyroid hormone as a result of low serum calcium levels. It is often seen in patients suffering from kidney disease.
Rights and permissions
About this article
Cite this article
Beenken, A., Mohammadi, M. The FGF family: biology, pathophysiology and therapy. Nat Rev Drug Discov 8, 235–253 (2009). https://doi.org/10.1038/nrd2792
Issue Date:
DOI: https://doi.org/10.1038/nrd2792
This article is cited by
-
Expression and Purification of FGFR1-Fc Fusion Protein and Its Effects on Human Lung Squamous Carcinoma
Applied Biochemistry and Biotechnology (2024)
-
Fibroblast growth factor-21 alleviates proteasome injury via activation of autophagy flux in Parkinson’s disease
Experimental Brain Research (2024)
-
FGF19 increases mitochondrial biogenesis and fusion in chondrocytes via the AMPKα-p38/MAPK pathway
Cell Communication and Signaling (2023)
-
Prospective use of amniotic mesenchymal stem cell metabolite products for tissue regeneration
Journal of Biological Engineering (2023)
-
Liver organoid culture methods
Cell & Bioscience (2023)